Compression Fractures

Minimally-Invasive Treatments Offer Promising – and Easier – Options to Patients
While procedures have been in place over the past 30 years to treat this condition, in recent years, much progress has been made with incorporation of minimally invasive approaches that allow the patient to resume a normal lifestyle as quickly as possible, and in many cases, by the next day.
The second most common reason people see a doctor is for back pain, and back pain can present in many ways and for a variety of reasons. Compression fractures are one such reason. The term alone sounds painful, and for many individuals, it has become a way of life. But it often doesn’t have to be that way. There are ways to treat compression fractures, but it is first important to understand what they are.
A compression fracture in the spine is usually caused by osteoporosis and is known as a vertebral bone that has lost up to 20% of its height due to the fracture. These fractures can occur in vertebrae anywhere in the spine but commonly present in the thoracic – or mid to upper region – of the back and they can also occur in the lower lumbar region.

While commonly referred to as a compression fracture, this type of abnormality is also known as a vertebral facture, wedge fracture or osteoporotic fracture. Compression fractures are typically associated with acute back pain (which can ultimately become chronic), loss of height, deformity, crowding of internal organs and loss of muscle due to lack of activity and exercise. Fortunately, because most of the damage from a compression fracture is limited to the front of the vertebral column, spinal cord or nerve damage is rarely associated with this event.
While procedures have been in place over the past 30 years to treat this condition, in recent years, much progress has been made with incorporation of minimally invasive approaches that allow the patient to resume a normal lifestyle as quickly as possible, and in many cases, by the next day.
A category of surgical procedures designed to stabilize a fractured vertebra with the goal of reducing the patient’s pain is called vertebral augmentation, generically termed as osteoplasty, and under that umbrella are two common procedures called vertebroplasty and kyphoplasty.
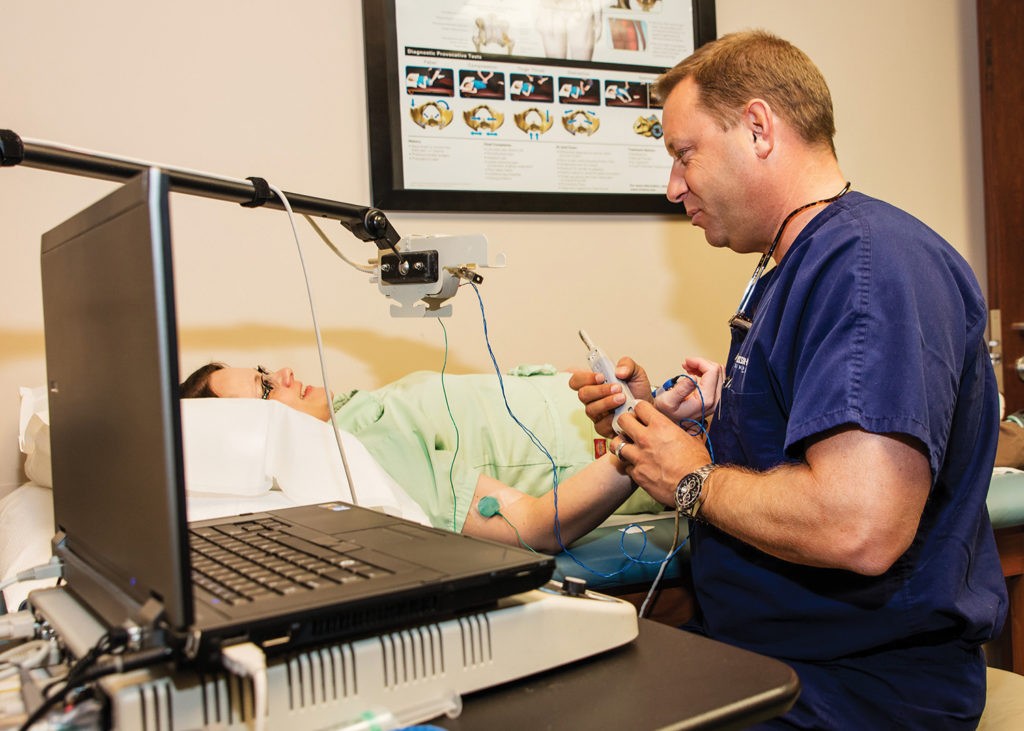
“These were designed for those individuals with compression fractures of the spine,” explained Dr. Constantine Lan Fotopoulos, board-certified physiatrist and specialist with Dickson-Diveley Midwest Orthopaedic Clinic. Specializing in minimally invasive and interventional procedures in the treatment of spinal disorders, Dr. Fotopoulos treats neck, back, hip, shoulder and knee pain and enjoys the rewards associated with assisting patients in overcoming pain and returning to the lifestyle they desire. Vertebroplasty/Kyphoplasty is one such procedure that truly excites him.
“I love doing these procedures,” emphasized Dr. Fotopoulos, who brings over 15 years of experience in this arena to the table. “The vast majority of patients feel much better the next day.”
Known for his motto of “never say never; never say always,” Dr. Fotopoulos cautioned that not every surgical intervention is 100% successful, but he does appreciate the growing opportunities for success rates with the changes in the approach to treating compression fractures and is far more optimistic about these newer modalities as opposed to the outlook patients realized years ago.
“Thirty years ago, a patient may have been doomed to bed rest as the only treatment for a compression fracture,” noted Dr. Fotopoulos. “Today, we can perform vertebroplasty in as little as 30 minutes or less under light anesthesia and with minimal recovery time. The patient may still feel some soreness in the back area after the procedure, as we did use a large needle, but after several hours, the pain should resolve itself.”
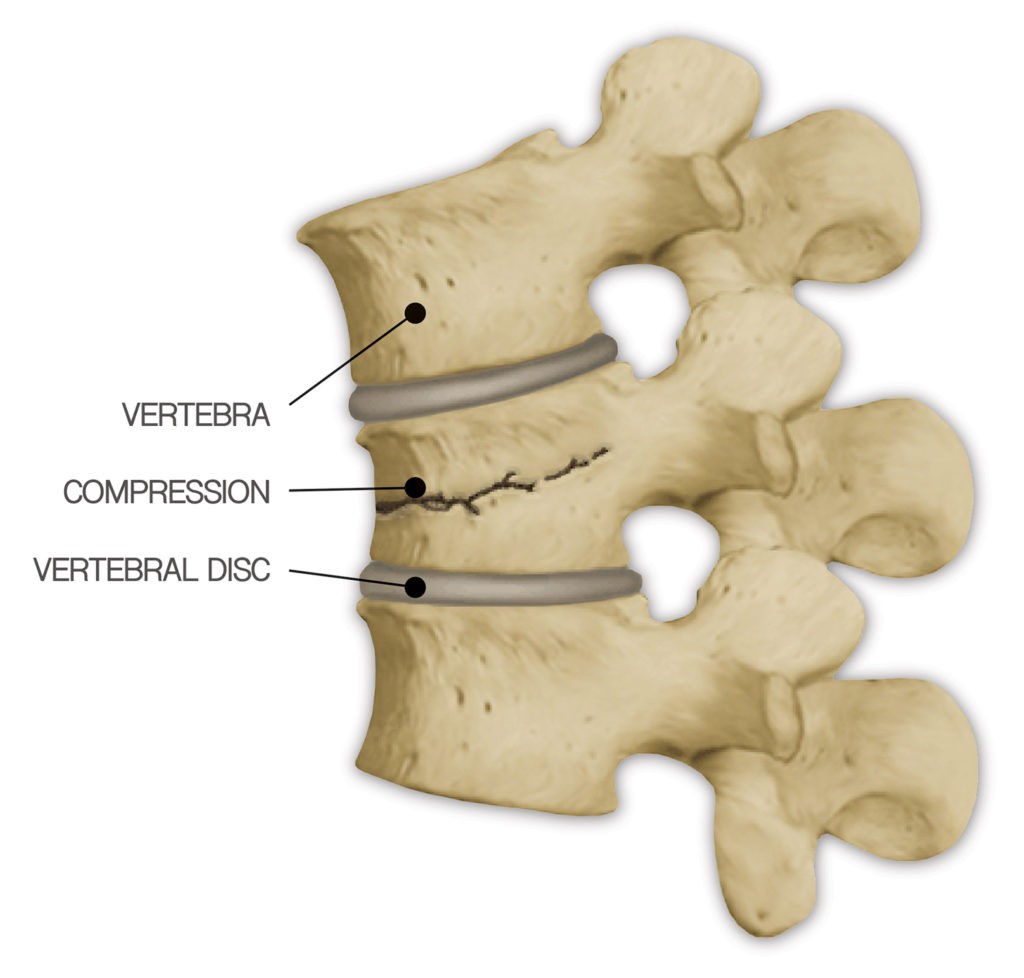
When a compression fracture occurs, the bone on the back bone is crushed, mainly due to the brittle nature of the bone, and the sheer weight causes it to crack. As a result, height is lost in that bone and pain ensues.
Dr. Fotopoulos explained the difference between vertebroplasty and kyphoplasty.
“Vertebroplasty, or vertebral augmentation, requires a large needle called a trocar that is placed through the fractured bone. We insert cement into the needle, essentially gluing or cementing the fractured pieces together so they can no longer move and the patient no longer feels pain in that area,” he said.
Kyphoplasty, on the other hand, uses a similar approach but with a balloon. Placed through the bone into the fractured bone via the trocar, a balloon is inflated, causing the fracture to open to its normal height in some cases. The balloon is then deflated, removed, and the pieces are cemented together as in the vertebroplasty.
For older women, compression fractures are often the result of osteoporosis, a disease known to cause thinning of the bone tissue and loss of bone density. Osteoporosis is not the only contributing factor to compression fractures, though. With frigid temperatures this winter leading to icy patches, a simple slip and fall can result in a fracture. Frequently, it can just be a simple move at the wrong time that creates a fracture.
“Even just standing up from a lounge chair can create a compression fracture,” said Dr. Fotopoulos.
With compression fractures, the pain usually presents as severe and limiting. However, some patients may experience no pain at all. While previously indicated the most common place for compression fractures to occur are in the thoracic and lumbar regions, for women, it often happens around the bra line, where a sharp, pinpoint pain may be realized upon bending over.
“Compression fractures in the cervical part of the spine are rare and more difficult to treat,” noted Dr. Fotopoulos, who explained that most compression fractures can be found in the T10, T11, T12, L1 and L2 areas.
For younger patients, a compression fracture can be the result of an accident, such as a skiing or boating mishap, and Dr. Fotopoulos sees numerous patients during the summer months as a result of such activities.
“With the younger patients, we expect those to heal and our standard approach in these cases is to brace them for six to eight weeks,” explained Dr. Fotopoulos. “For older patients, the brace can become uncomfortable and leave them feeling irritable, which is why many of these people opt for the procedure.”
Even though osteoporosis of far more common in women, Dr. Fotopoulos advised it can occur in men. However, the problem with such a related fracture is that it is not always properly diagnosed and frequently the pain is thought of as general back pain, such as from a muscle strain or some other type of soft tissue injury, or even just an expected part of aging. As a result, though, many vertebral fractures may go undiagnosed and not treated.
To ensure the exact cause of the back pain, Dr. Fotopoulos always does his due diligence before each procedure.

“I feel it is my responsibility to rule out the possibility of other issues, such as cancer,” stressed Dr. Fotopoulos, whose typical standard operating procedure includes conducting a biopsy with each case prior to surgery. “We always obtain an MRI before procedures, too. For those who cannot undergo an MRI, we do a bone scan or a CAT scan to help with our diagnosis of a compression fracture. These options are far better than a standard x-ray.”
With an MRI, Dr. Fotopoulos can determine the age and status of the fracture and whether or not a procedure would be a viable option. Incorporating this approach prior to the procedure is an integral part of Dr. Fotopoulos’ attention to detail when it comes to treating his patients.
Further, Dr. Fotopoulos warns that when a patient sustains a compression fracture, there exists the chance of a follow-up one.
“Having a previous compression fracture results in a 25% chance of another one within the next 12 months,” stated Dr. Fotopoulos, stressing that the easy part is treating it. “Afterwards, we have to make sure the underlying cause is treated appropriately to reduce the risk of more fractures.”
Post-surgical treatments may include physical therapy to assist with gait and balance and/or the patient may require a change in medication for osteoporosis.
If back pain is troubling you, then perhaps a call to Dr. Fotopoulos may just be your answer. Don’t let fear get in the way. As opposed to 30 years ago, these procedures are faster, require less parts, and in some cases can even be accomplished through the use of local anesthesia.
“It’s probably no worse than getting a cavity filled,” smiled Dr. Fotopoulos.
For more information on Dr. Fotopoulos, Dickson-Diveley Midwest Orthopaedic Clinic or verterbroplasty/kyphoplasty, go online at dd-clinic.com or call 913.319.7600. Offices are located in Leawood, Kansas and at St. Luke’s Hospital in Kansas City, Missouri.



