Pain. That’s a four-letter word with which no one wants to make friends, but the Institute of Medicine reports that 100 million people in the United States suffer from chronic pain, and supporting research of that phenomena suggests this costs the American population an estimated 515 million workdays each year, generating nearly 40 million visits to physicians annually. That also equates to approximately $100 billion per year in lost work time and health care expenses.
Typically speaking, when someone is dealing with chronic pain, they will usually turn to treatments such as prescription painkillers, which often prove to be an inadequate measure by which to treat the pain. However, a recent FDA-approved device that has been used in Europe and Australia for the past seven years is showing promising results with respect to treating chronic pain.
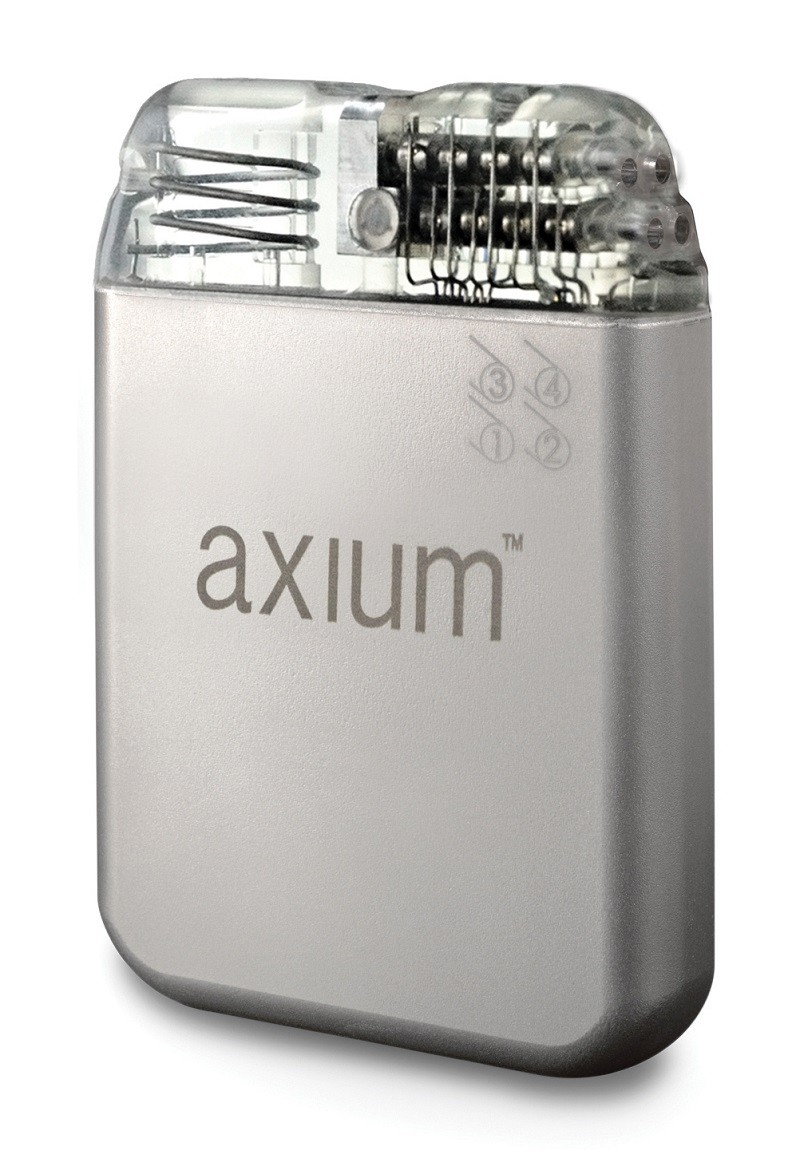 Dr. Constantine Fotopoulos, a specialist in interventional spine and sports medicine at Dickson-Diveley Midwest Orthopaedic Clinics, is one of only 300 physicians in the United States who has been specifically appointed by St. Jude Medical, Inc., a global medical device company and international leader in the development of therapies for the treatment of chronic pain, to be trained with the use of the newly approved St. Jude Medical Axium Neurostimulator System. Clinically described, this system “targets the dorsal root ganglion (DRG), a spinal structure densely populated with sensory nerves that transit information to the brain via the spinal cord.” This device allows for spinal stimulation that can target specific areas of the body where pain occurs.
Dr. Constantine Fotopoulos, a specialist in interventional spine and sports medicine at Dickson-Diveley Midwest Orthopaedic Clinics, is one of only 300 physicians in the United States who has been specifically appointed by St. Jude Medical, Inc., a global medical device company and international leader in the development of therapies for the treatment of chronic pain, to be trained with the use of the newly approved St. Jude Medical Axium Neurostimulator System. Clinically described, this system “targets the dorsal root ganglion (DRG), a spinal structure densely populated with sensory nerves that transit information to the brain via the spinal cord.” This device allows for spinal stimulation that can target specific areas of the body where pain occurs.
With this brand new device, physicians can provide effective pain relief to patients with certain neuropathic conditions that otherwise might not be achieved by traditional spinal cord stimulations. This is an ideal procedure for someone who has tried numerous treatment options yet has failed to obtain sufficient pain relief.
“The perfect candidate for this procedure is someone who is experiencing unrelieved pain from such conditions as previous knee surgery; pain after knee replacement surgery; unresolved pain issues from foot and ankle surgeries; post-hernia pain or hip replacement surgery,” noted Dr. Fotopoulos. “This procedure allows localized stimulation, treating complex regional pain syndrome, also known as sympathetic dystrophy.”
The DRG is a small bundle of nerves responsible for transmitting pain message to the brain, controlling when sensations can enter your spinal cord. Every vertebra in the spine has a DRG.
Through the use of DRG stimulation, leads are implanted under the skin in the spine. Mild electrical impulses are sent to the area of a DRG within the spine, which allows the DRG to block pain signals from traveling to the brain from that specific area. As a result, instead of the sensation of pain, a patient may sense either a slight tingling feeling or the complete absence of pain.
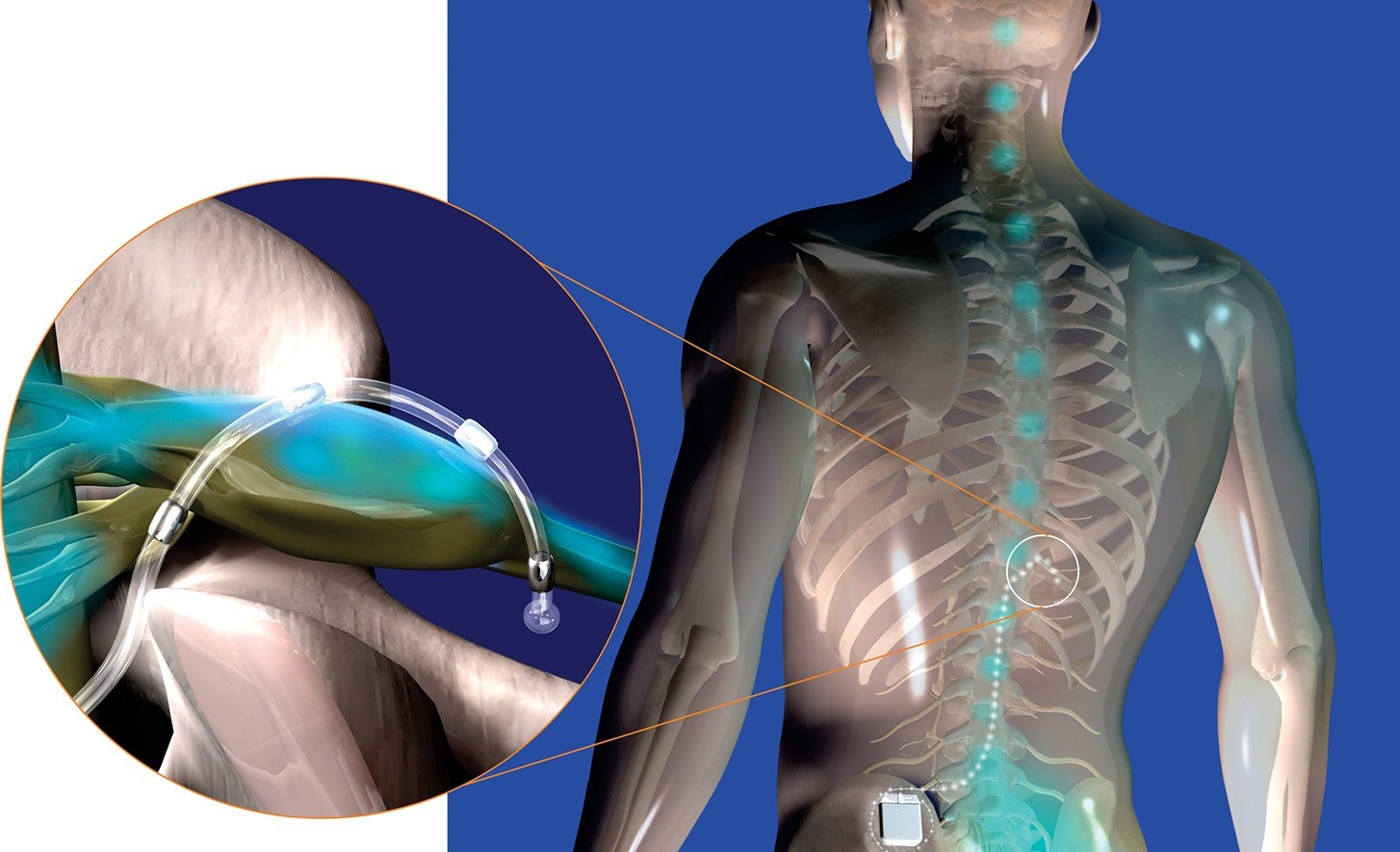
Procedurally, this device is easily navigated by a trained physician. A lead is implanted on the nerve that is attached to the DRG through which the electrical impulses are sent, powered by a battery that is also implanted beneath the skin. Much like a spinal cord stimulator, it is operated by a rechargeable battery and is implanted through a device that goes through the skin. DRG stimulation can be directed to certain areas from which the pain is felt. DRG simulation aids in reducing effects from problems such as continued pain after a total knee or hip replacement, post-amputation pain, pain after hernia repair and complex regional pain syndrome.
 It should be noted, however, that this type of stimulation is not promoted as a cure for the source of pain, as pain reduction varies by individual. Most patients, however, experience at least a 50% reduction in pain, with some studies showing as high as 90% reduction in pain.
It should be noted, however, that this type of stimulation is not promoted as a cure for the source of pain, as pain reduction varies by individual. Most patients, however, experience at least a 50% reduction in pain, with some studies showing as high as 90% reduction in pain.
Done on an out-patient basis under light intravenous sedation in typically under an hour, an initial trial procedure is first required. Patients may realize minor post-surgical pain but can expect to return to their normal routine almost immediately.
The use of the stimulator can result in decreased pharmaceutical requirements; less side effects; and additionally offers more long-term pain control. With both two and five-year data reports published, the company behind the device has reported upwards of an 80% success rate.
“After researching all of the data, I am excited to offer it to my patients,” expressed Dr. Fotopoulos. “In all rights, it should nearly abolish the rare and severe pain seen after knee replacement surgeries. Bear in mind, it is not the norm to have pain (in this regard) but it is common. Further, no single device helps everyone, as pain is subjective.”
By having the opportunity to offer this therapy to his patients, Dr. Fotopoulos now has a more expansive portfolio of treatment options for patients suffering from a wide range of chronic pain conditions.
“Sure, you could do in-office cryotherapy to stun the nerves, but this procedure is definitely the hammer. It has a significant positive outcome and is truly impressive,” noted Dr. Fotopoulos.
C. Lan Fotopoulos, M.D.
Dickson-Diveley Orthopaedics
2 Locations
- Saint Luke’s Hospital Campus Medical Plaza Building 1, Ste 610, 4321 Washington St., KCMO
- 3651 College Blvd., Leawood, KS 66211
913.319.7600
DD-Clinic.com



