Peace of Mind

Written by Ann E. Butenas
With its highly advanced Level III Neonatal Intensive Care Unit, University Health provides highly specialized care for moms and babies should complications arise.
 If you have ever wondered about the significance behind University Health (UH), perhaps its vision speaks loudest: leading the way to a healthy community. That is accomplished through very strategic planning, specific partnerships, and experienced people who help lead the charge in very comprehensive, thoughtful, and inspiring ways.
If you have ever wondered about the significance behind University Health (UH), perhaps its vision speaks loudest: leading the way to a healthy community. That is accomplished through very strategic planning, specific partnerships, and experienced people who help lead the charge in very comprehensive, thoughtful, and inspiring ways.
Kansas City’s major funders embraced the vision and came through with leading grants from not only the Sunderland Foundation but also the Hall Family Foundation.
An academic center that provides quality healthcare to the metro area and beyond, regardless of insurance status, UH is a two-hospital system serving residents of Jackson County and Kansas City, MO. Its doctors, in affiliation with the University of Missouri-Kansas City (UMKC) School of Medicine, teach, guide, and inspire the doctors of the future. This is further enhanced by staying ahead of medical advances, giving cutting-edge care to patients, and providing the utmost in innovative education to the medical students.
Because it is an academic medical center, UH has the ability and capacity to handle some of the most complex healthcare cases. Academic medical centers combine education, research, and clinical care to provide the optimum in health care with advanced technology and expertise for all patients. In fact, the organization recently rebranded itself assuming the name University Health to showcase that partnership with the school of medicine and to recognize the huge advantage that partnership brings to our patients. Among those advantages is the hospital’s new and technologically advanced Level III Neonatal Intensive Care Unit (NICU).
Kansas City’s Only Essential Level III Neonatal Intensive Care Unit
 With just 5,000 square feet of space, the original Level III NICU at UH was built in 1976, the same year the hospital was built. It’s safe to say a lot of babies have been born since that time. Lately the demand for Level III NICU services has increased by almost 20%. On most any given day, each of the 19 incubators in the original unit were in use, providing the necessary life-sustaining care for the smallest, weakest, and sickest of babies.
With just 5,000 square feet of space, the original Level III NICU at UH was built in 1976, the same year the hospital was built. It’s safe to say a lot of babies have been born since that time. Lately the demand for Level III NICU services has increased by almost 20%. On most any given day, each of the 19 incubators in the original unit were in use, providing the necessary life-sustaining care for the smallest, weakest, and sickest of babies.
It was becoming increasingly evident a larger footprint was needed to facilitate and support the increase in demand for patient care and family privacy. Plus, as the new generation of technology and state-of-the-art equipment was incorporated to help for the growing number of patients, the available accommodating space would have to expand. As a result, the funding request was to raise $18.8 million for the expansion and renovation of Kansas City’s only essential Level III NICU.
“The foundation is responsible for rallying community support,” emphasized Charlie Shields, CEO of UH. “We have an $18.9 million capital campaign that was privately started in 2018 and went public in 2019. Thanks to a $10 million gift from the Sunderland Family Foundation that year, we were able to tell our partnership story with UH and Children’s Mercy Hospital (CMH) to our donors. Our community saw the need for a major investment in moms and babies.”
Delivering Miracles was the name of the fundraising campaign.
“Funders could walk through a cramped NICU and knew it needed so much more,” noted Shields. “But fundraising was just one component. The compelling story is that this expansion defines our connection to, and partnership with Children’s Mercy Hospital and its leading-edge children’s research center.”
Kansas City’s major funders embraced the vision and came through with leading grants from not only the Sunderland Foundation but also the Hall Family Foundation.
“We can now provide private space for moms and families who are often with us for weeks of intensive care,” said Shields.
The 20,000 square foot space also supports long-term expansion of neonatal technology and staff to meet growing needs.
“It is critical that we provide a unit that can accommodate changing technology and continue to attract the best and brightest medical staff,” expressed Shields.
The staff and the equipment at UH are prepared to care for babies born prematurely, with other issues, and with multiple births. It’s no wonder it is a referral center for those with at-risk pregnancies from around the region. The NICU now offers 29 beds, giving each baby and family their own private suite. Further, UH and Children’s Mercy Hospital (CMH) are all part of a collaborative in shared OBGYN space.
UH is intermingled in this community and is a vital organization essential to providing care to the underserved and those with insurance resources. UH is blessed with a community that recognizes the value the organization brings to the community and supports in so many ways, including financially.
Years in the making, this NICU renovation reflects the commitment and trust the surrounding community has in UH and the services it offers patients and families. The new NICU is an outstanding place for babies who need the best level of care and to help babies get the great start they deserve.
Thanks to generous donors, now the tiniest of patients and their families have something spectacular to enjoy, a new state-of-the-art NICU that opened in 2022. Babies and their families can now move into their new home at UH and appreciate its beautiful surroundings and all of the amazing technology it offers to deliver the best in-class patient experience available. There are new isolettes, ventilators and monitors, all interconnected and able to communicate to each other. The integrated technology at this newly expanded and renovated NICU is an amazing tool that does its job without getting in the way of babies and their families.
One young mother gratefully expressed her appreciation for the NICU, the staff, and the medical providers.
“I had a high-risk pregnancy and delivered early,” she recalled. “Every doctor, nurse, and assistant treated me with so much kindness and support. They are all very knowledgeable and really made me feel like family. I have had such a wonderful experience here at University Health.”
The new facilities at UH now truly enhance the already outstanding care patients and their families receive at this facility. When a baby has to be in a NICU, it should be in a place that makes you feel comfortable, loved, and cared for.
The Bridge of Hope: 63 Steps to Peace of Mind
 An added benefit for the moms who deliver at UH Truman Medical Center (TMC) is the connection the hospital has to CMH. Crossing a footbridge called the Bridge of Hope that connects both hospitals, it takes just 63 steps to CMH from UH to enjoy immediate access to its Level IV NICU should mother or baby need it. This is where the highest level of care can be found for premature and critically ill newborns. When every second matters, this bridge creates seamless access to critical care at a time when it is urgently needed. UH is the only hospital in the metro area that has this physical connection.
An added benefit for the moms who deliver at UH Truman Medical Center (TMC) is the connection the hospital has to CMH. Crossing a footbridge called the Bridge of Hope that connects both hospitals, it takes just 63 steps to CMH from UH to enjoy immediate access to its Level IV NICU should mother or baby need it. This is where the highest level of care can be found for premature and critically ill newborns. When every second matters, this bridge creates seamless access to critical care at a time when it is urgently needed. UH is the only hospital in the metro area that has this physical connection.
 Maternal Fetal Medicine
Maternal Fetal Medicine
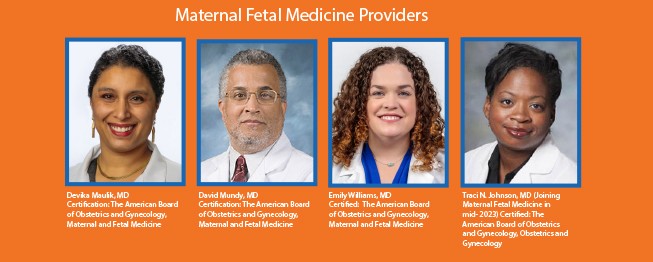
A sub-specialty of obstetrics, Maternal Fetal Medicine (MFM) focuses on both the diagnosis and the treatment of expectant mothers and their unborn babies. This specialty is also known as perinatology and helps in managing the health issues of both moms and their babies prior to, during, and shortly after pregnancy. MFM physicians earn this subspecialty designation within the field of obstetrics.
Provider profile: Dr. Devika Maulik
Dr. Maulik has an obvious passion for MFM. Her strong training and medical background acquired from other academic centers are a tremendous asset to this practice. Since she has returned to UH, this group of providers has been able to successfully expand and grow the Maternal Fetal Medicine practice.
Well-trained in top academic settings, Dr. Maulik attended medical school at Cornell Medical School, followed by a Fellowship at the University of Missouri – Kansas City. From there she completed her residency at the University of California, Los Angeles and subsequently did her internship at New York Presbyterian Hospital. But her ambitions did not stop there.
With a sub-specialty in Maternal Fetal Medicine (MFM), Dr. Maulik is a specialist in high-risk pregnancies. This is an area of practice that requires additional training above and beyond the residency and training completed to become an OBGYN.
“To obtain an MFM, you have to complete three additional years of study within this subspeciality,” indicated Dr. Maulik, who is dual Board Certified by the American Board of Obstetrics & Gynecology in OB/GYN and MFM. Her father actually started the MFM Department, so Dr. Maulik continues the legacy of this family business with a strong commitment to service.
“We have a wonderful team of physicians and experienced academic doctors here, all of whom keep up to date on best practices,” emphasized Dr. Maulik. “Because of that, moms get great care from the team. When treated in a teaching hospital like ours, patients realize better outcomes.”
According to Dr. Maulik, the nursing staff is an equally integral part of this well-oiled machine. Because they are experienced in taking care of high-risk pregnancies, the nurses are more in tune to any concerns that might arise, and they can therefore tailor their care for those specific pregnancies as needed.
In addition to the experienced clinicians, patients receive support through state-of-the-art technology and the specialists who work in this realm.
“With maternal fetal medicine, technicians complete rigorous training in ultrasound, developing their skills to a very high level,” said Dr. Maulik. “They are an integral part of pre-natal care, making sure everything looks anatomically correct. We also have a state-of-the-art ultrasound suite here and are recognized as one of the best places to get a pre-natal scan.”
With the updated facilities, Dr. Maulik indicated that if a patient is experiencing a high-risk pregnancy with the suspicion the baby may require NICU support and other specialized services, the mom is not separated from the baby under these circumstances.
“The newly updated facilities make this the best place possible for these situations,” said Dr. Maulik, “ and they allow us to recruit and retain highly trained Maternal Fetal Medicine staff to care for our patients.”
Dr. Maulik further emphasized that the neonatology team at CMH has a long-standing relationship with them, making UH TMC the best place to deliver a baby if a patient needs such specialized services.
“The neonatologists and the MFM doctors work between the two hospitals, and some of our specialists practice at Children’s Mercy, so there is a lot of cross talk between the two teams,” explained Dr. Maulik. “Plus, a routine pregnancy can turn into a high-risk event. I tell people pregnancy is a normal part of one’s reproductive health if they choose to get pregnant. However, it is also a stress test which can result in complication on the mom’s body and can also result in complications for the baby.”
Also included among the hospital’s expert diagnostic services are first trimester screening, cell-free fetal DNA screening, fetal echocardiography, amniocentesis, evaluation, and management of pregnancies complicated by medical conditions, and preconceptual counseling.
 Provider profile: Dr. Traci Johnson
Provider profile: Dr. Traci Johnson
Dr. Johnson was an OBGYN at UH Women’s Care at Lee’s Summit for many years, and UH is excited about her return to the practice in mid-2023 after completing a subspecialty in MFM. Her return is welcomed by staff who trust her and by patients who appreciate her patient focus and advocacy.
“I loved caring for patients as an OBGYN. However, as the general population is developing more chronic conditions and presenting with pregnancy with less healthy overall status, it was becoming increasingly necessary to obtain additional training,” expressed Dr. Johnson.
Dr. Johnson emphasized how UH stands out as a strong leader among other MFM practices in the metro compared to other practices that offer MFM in that this is the only practice in our region able to meld together the following:
- quaternary care for the mother/fetus dyad (able to offer low-risk pregnancy care all the way up to fetal interventions)
- expertise in complex surgical cases such as those patients with different anatomy, colostomies, prior surgical complications, and placenta accreta spectrum
- expertise in caring for those with the very best insurance, and those with no insurance at all, as well as special populations (patients with disabilities, special cultural considerations, and emigrating from a variety of different countries)
- state of the art NICU with neonatologists that staff both our NICU and the higher level NICU at CMH linked by the Bridge of Hope
- advanced Behavioral Health resources with psychiatrists and psychologists who specialize in the most complex psych disorders.
- diverse clinical staff and administration focused on ensuring patients’ needs are met in an equitable, inclusive way.
For more information on University Health Maternal Fetal Health, visit them
online at https://www.uhkc.org/high-risk-pregnancy/
Clinics located at:
University Health Women’s Care Obstetrics and Gynecology (UH 1)
2101 Charlotte, KCMO | 816-382-6169
University Health Women’s Care Lee’s Summit
3450 Ralph Powell Road | 816-382-6170
 University Health Women’s Care
University Health Women’s Care
Truman Medical Center Birthplace
2301 Holmes Kansas City, MO 64108







