After COVID-19 Strikes

Managing the Road to Recovery
While most people who get COVID-19 are likely to recover without a host of long-term effects, a small percentage of patients with severe symptoms can suffer from long-term health impacts.
For the past several months, it’s a safe bet to assume all of us have at one time or another wondered if that random sneeze, scratchy throat, mild cough, or nagging headache were signaling the start of something more than just the common cold or flu bug. Ever since the novel coronavirus has stolen the healthcare spotlight, we have been warned to protect ourselves through diligent hygiene, shelter-in-place orders, masking and social distancing measures, as well as to remain on the lookout for any possible symptoms and to self-quarantine as necessary.
Contracting the novel coronavirus is frightening enough. While many people do recover with minimal issues, there are patients whose battle with this virus completely changes the trajectory of their lives, requiring long-term hospitalization, and, in some cases, if they did not succumb to the virus, the need to be placed on a ventilator for extended periods of time. As a result, these patients’ lives and health have been upended, leaving them on the receiving end of requisite continued medical care but perhaps not in a place most conducive to such continuity of care.
Fortunately, MidAmerica Rehabilitation Hospital (MARH) in Overland Park, Kansas, rose to the challenge and opened its doors to COVID-19 patients, providing a place of rehabilitation, respite and multiple therapeutic measures necessary to get these individuals back in the recovery lane and headed back home.
As part of the Encompass Health system, a nationwide provider of post-acute healthcare services, MARH is one of 127 hospitals in the country. It assists patients in regaining their independence after a life-altering illness or injury. In response to the recent pandemic, MARH developed a COVID unit to rehabilitate patients recovering from COVID-related pneumonia.
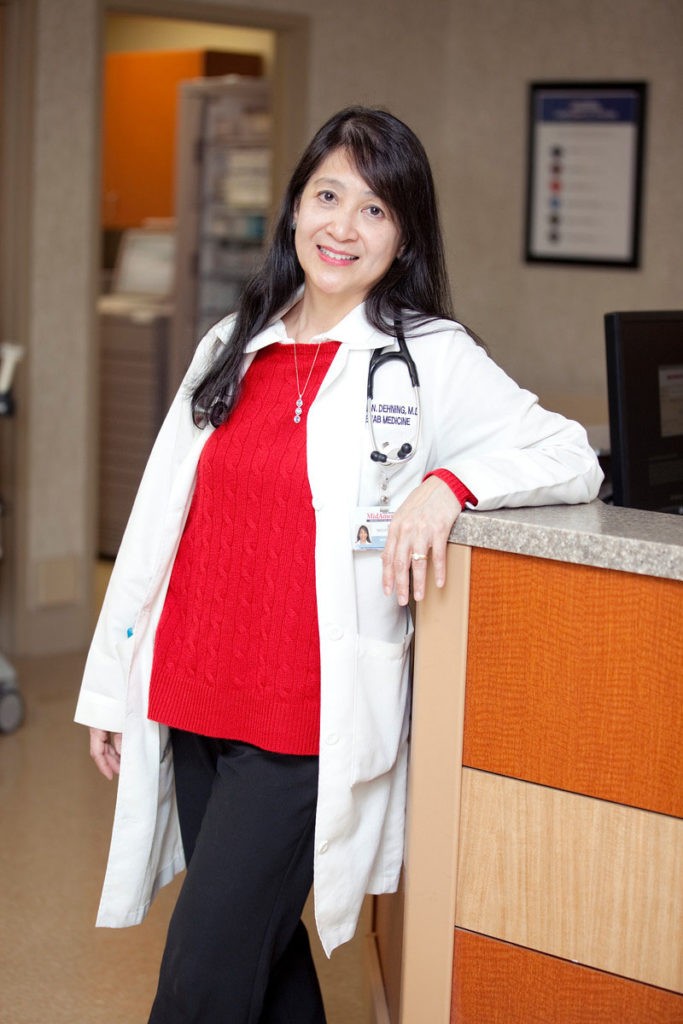
“We were one of the first rehabilitation hospitals to accept COVID-19 patients in the Kansas City area and beyond,” indicated Dr. Cielo Navato-Dehning, Medical Director of MARH. “Early on, we made the decision to take part in helping care for critically ill patients to help relieve the burden on the acute hospitals.”
MidAmerica Rehabilitation Confidently Mobilized Its Forces
Realizing there was a need to get patients into intensive rehabilitation, the health professionals at MARH went into action to be prepared. The demand for intensive rehabilitation for COVID patients was highly apparent, after consults began arriving from local acute care hospitals.
“We all pulled together and had a big team before we even knew it,” indicated Dr. Navato-Dehning. “We had many volunteer therapists and nurses, and it sort of just become a big, spirited thing!”
The patients for whom they have cared, ranging from ages 35-93, have typically come into the facility often lacking the ability to independently sit up; are still coughing; have muscle aches; and are classified as critically ill. Some have been in the ICU and on ventilators for many days and have come to MARH to work on one of their biggest struggles to date with this virus: simply breathing. Pulmonary rehabilitation is part of the recovery process, as COVID-19 is an illness that frequently targets the respiratory system.
“These recovering patients have come off oxygen and have been weaned from multiple medications. To see how they recover in rehab is so rewarding,” noted Dr. Navato-Dehning. “They transition from not being able to even comb their hair to successfully walking up and down stairs.”
Addressing other impacts of COVID-19
Aside from the physical aspect of this health challenge, many patients suffer from psychological impacts. Some are not even aware of how long they have been in the hospital, and a certain condition related to COVID-19 may present.
“There is a distinct condition called encephalopathy with this virus that causes damage to the brain, most specifically to the frontal lobe,” explained Dr. Navato-Dehning. “When patients come out, it is difficult for them to concentrate, and many don’t remember much prior to becoming ill.”
While Dr. Navato-Dehning and her peers still question if this is a direct result of the virus, the answers do not readily appear.
“This is a novel virus with which we have no experience, but it is showing that with the critically ill, something has changed in the brain,” she noted.
One 60-year-old patient who was rehabilitated at MARH did not hold back with respect to her feelings about the severity of this virus. She warned, “If people have any doubts about gathering in large groups or any doubts about this virus at all, they should talk to me!”
Another recovered patient, a 45-year-old front line provider, was hit with COVID-19 and nearly lost his life to the virus. “He spent six weeks in the hospital and then he came to us,” recalled Dr. Navato-Dehning. “When he first arrived here, he was struggling to stand.”
Under the care of MARH, most patients, like these mentioned, return home in about two to three weeks.

Recovery from the emotional impact
Dr. Navato-Dehning also emphasized issues beyond the physical. “These patients have been in the hospital, isolated and with no visitors allowed,” she commented. “The isolation they felt has made them sad and fearful, and there is no doubt it has affected them psychologically.”
Dr. Navato-Dehning and the team at MARH, however, are always on full throttle with enthusiasm and positivity, offering round-the-clock emotional and physical support for the patients in a way that makes them strive even harder for the ultimate goal: returning home.
Fully protected / full trained
While at times it may seem as if the coronavirus is lurking behind every corner, we can all take measures to keep it at bay. However, the medical team at MARH is prepared.
“We are always fully protected and are highly trained to care for these patients,” indicated Dr. Navato-Dehning. “We know the CDC guidelines and know how to wear the PPE (personal protection equipment) and are consistent about it. We do take this situation very seriously.”
Even though Dr. Navato-Dehning does not describe her team as the faces of the frontline, they do play a highly integral role in this battle against the virus.
“We’re more like the generals, behind the lines yet equally important,” she explained. “We serve the community by helping with rehabilitation efforts, leaving more open beds in the hospitals. We provide intensive therapy three hours a day and help these patients to feel themselves again so they can get off the oxygen and go home.”
One of the patients assisted by MARH who was struck by the virus earlier this year ended up on a ventilator. Her husband also contracted the virus, but unfortunately, did not survive.
“She was in her mid-60s and believes she contracted the virus while at a funeral in February,” indicated Dr. Navato-Dehning. “She recalled the pastor coughing a bit during the service and believes that is how it started.”
Another couple received successful rehabilitation at MARH.
“A husband, wife and their son got sick,” said Dr. Navato-Dehning. “We took the wife first and then ended up taking care of her husband. Their son made it home without intervention from us but now all three are back home. Everyone is different with their story of how this virus affects them.”
Even for people who have officially recovered, feeling completely back to normal may take an appreciable amount of time. Improving health and strength after COVID-19 requires a team effort.
For more information on Dr. Cielo Navato-Dehning and MidAmerica Rehabilitation Hospital, call 913.667.7505 or visit midamericarehabhospital.com






