Ask The Doctor
Stroke with Dr. Cherie Suther
Stroke is a medical emergency that occurs when the blood supply to part of the brain is interrupted or reduced, preventing brain tissue from getting oxygen and nutrients. In the time it takes to read this article, at least one person in the U.S. will die from a stroke. Depending on how fast you read, 10 or more will suffer a stroke before you reach the last sentence. Stroke, obviously, is nothing to take lightly.
The Centers for Disease Control and Prevention estimate that stroke kills about 140,000 Americans each year. That is about 1 of every 20 deaths that occur annually in the country. Someone in the U.S. has a stroke every 40 seconds, and someone dies from it every four minutes.

We had the honor of speaking with Dr. Cherie Suther, Stroke Program Director at MidAmerica Rehabilitation Hospital in Overland Park, Kansas to find out more information about what to look for when you think you or a loved one is having a stroke and what the treatment plan looks like post-stroke.
Dr. Suther has been at MidAmerica since 2012, did her internship at St. Louis University Hospital and residency training in the specialty of rehabilitation medicine at the University of Kansas.
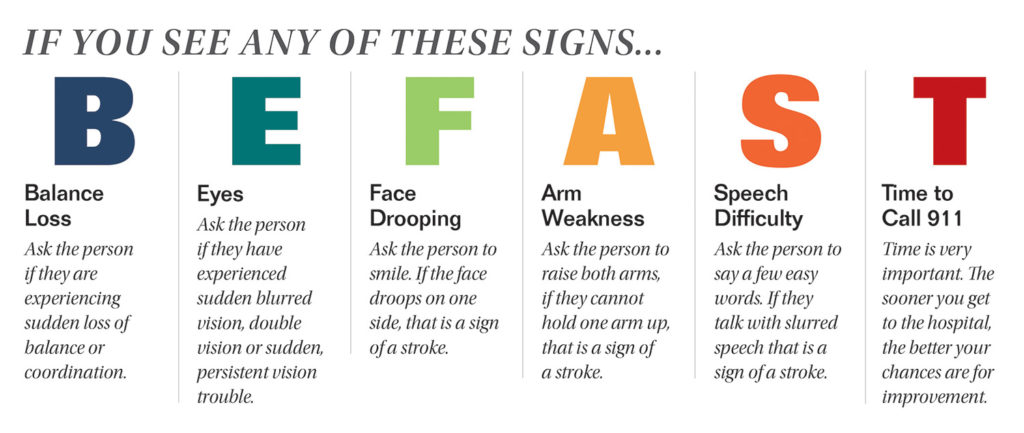
What are the signs of a stroke?
It is important to recognize the signs of stroke early. Learning the early signs of a stroke can prevent further damage to the brain, major disabilities, or even death. It is very important to dial 911 as soon as you recognize the signs of stroke in yourself or another person.
Your doctor will diagnose your stroke based on your signs and symptoms, and your medical history. Common diagnostic tools for stroke are medical imaging tools such as Brain Computed Tomography, Magnetic Resonance Imaging, and Carotid Ultrasound.
Tell us about the different types of strokes and how they present.
A stroke in general is the sudden interruption or loss of blood supply to the brain. Both can present with the symptoms I mentioned above. There are two kinds:
Ischemic Strokes – About 80% of strokes fall in this category. This type of stroke happens when blood flow through the artery that supplies oxygen-rich blood to the brain becomes blocked.
Hemorrhagic Strokes (Bleeding Strokes) – A smaller percentage of strokes fall in this category. In this type of stroke an artery in the brain leaks blood or ruptures and floods the brain tissue with blood. The leaked blood puts too much pressure on brain cells, which damages them. There are 2 subtypes of hemorrhagic stroke: 1) intracerebral hemorrhage, which occurs when an artery in the brain bursts, flooding the surrounding tissue with blood and 2) subarachnoid hemorrhage, which occurs when there is bleeding in the area between the brain and the thin tissues that cover it.
In addition to the two major types of stroke, there is another type called a transient ischemic attack (TIA) also known as a mini-stroke. In this type blood flow to the brain is blocked for only a short time — usually no more than 5 minutes. This limits the damage that is done to the brain.
What are the treatment plans for strokes?
There are 3 treatment stages for stroke. The first part is prevention. Therapies to prevent a stroke are based on treating an individual’s risk factors such as diabetes, high blood pressure, and atrial fibrillation. Acute stroke therapies attempt to stop a stroke while it is happening by dissolving a blood clot of an ischemic stroke or by stopping the bleeding of a hemorrhagic stroke. Again, early intervention is extremely important. For instance, during an ischemic stroke there is a small window of 3 hours to have a drug called tPA administered in the hospital. Also known as a “clot buster”, tPA dissolves artery obstructing clots. When stroke patients receive tPA they are at least 30 percent more likely to recover from their stroke with less disability after 3 months than those who do not receive it.
What we focus on here at MidAmerica, is Post-Stroke rehabilitation, including physical therapy, speech therapy, occupational therapy and more. Continuing to manage those medical risk factors, such as high blood pressure, is also an important part of the patient’s functional recovery.
What does recovery and quality of life look like in a typical patient?
Every patient is different. The timetable of recovery depends on the type of stroke that the patient had, as well as other medical complications that may be present. However, because of extensive data over the years, we DO know that most recovery that will take place will happen over the first six to twelve-month period. This period is crucial. If the patient participates in an acute in-patient rehabilitation program, we also know that is very beneficial. I also tell my patients that it doesn’t just stop after 12 months, the recovery process is still important and you will continue to have healing components in the brain. It’s an amazing organ.
Do genetics play a role?
Genetics in terms of risk factors and family history does play a role, of course. It’s important for patients to do as much as they can to reduce those risk factors to prevent a stroke. Living a healthy lifestyle, eating right, and not smoking are critical to prevention.
What support groups are available?
It is one of the things that we are really proud of here at MidAmerica. We do a monthly stroke support group which provides an opportunity for our patients and families to come together and talk about how their recovery process is going and ask questions. The American Stroke Foundation is another great resource for survivors and their families. Our stroke program also participates in the Stroke Walk and Cycle Nation, two amazing fundraising opportunities to help in the fight against stroke.
For more information on Dr. Cherie Suther and MidAmerica Rehabilitation Hospital call 913.491.2400 or visit MidAmericaRehabHospital.com






