Combating Hepatitis
Interventions for a Healthy Future
As World Hepatitis Day approaches July 28, 2017, health officials and policy makers work to bring greater awareness to an often underinformed, and misinformed public. Lack of knowledge shrouds viral hepatitis in mystery which has put it at the top of the list as leading cause of death worldwide, ahead of even the scourge of aids.
Hepatitis Should Be Front Page News
Most people do not know that there are five hepatitis viruses – A, B, C, D and E. Nor are they aware how each is contracted, or which they might most commonly encounter when and where they live and travel. Most believe that hepatitis is nearly exclusive to poorer nations with limited medical care. While the incidents are higher in countries with limited medical care, it is not eliminated in the United States. In fact, the numbers affected by hepatitis A, B and C in the United States all increased in 2015, according to the most recent data.
HAV, HBV, and HCV are endemic to the US, and responsible for more than 90% cases of acute hepatitis. Hepatitis A is the most common cause of acute hepatitis, while hepatitis C is the most common cause of chronic hepatitis. Although they have similar symptoms, they have different modes of transmission and affect the liver differently.
Hepatitis Is Not Worlds Away
Typically, the public views hepatitis as affecting someone else, somewhere else. Recent headlines have brought the virus closer to mind, and a lot closer to home. Recently, a hepatitis outbreak in San Diego County California saw 160 reported cases, 120 hospitalizations, and four deaths. According to the Centers for Disease Control, hepatitis A is primarily spread when someone who has never been infected or vaccinated for HAV ingests food or water contaminated by the waste of an infected person. It is rarely fatal, according to published literature. In the San Diego cases, the virus was not linked to a single source but many of the infected individuals were homeless and/or used illegal drugs. In this case, it proved to be very lethal.
The Hilo Fish Company began recalling tuna in Oklahoma, Texas, and California when Yellowfin Tuna samples from Indonesia tested positive for the virus May 18, 2017. Though there have been no known cases of HAV stemming from the recalled frozen tuna, it was distributed to restaurants within the three states and likely in use before the testing.
In December of 2016, the United States saw a multi-state outbreak of hepatitis A linked to frozen strawberries. In this instance, one hundred forty-three people were infected in nine states.
70 Million People Have Been Vaccinated
Vaccines exist for the hepatitis A and B viruses. Hepatitis A vaccines were recommended in the US beginning in 1996 and since that time the number of reported cases each year has dropped from 31,000 cases to fewer than 1,500.
Although over 70 million people in the United States have been vaccinated against the hepatitis B virus, there are an estimated 847,000 people with evidence of infection according to the latest National Health and Nutrition Examination Survey (NHANES).
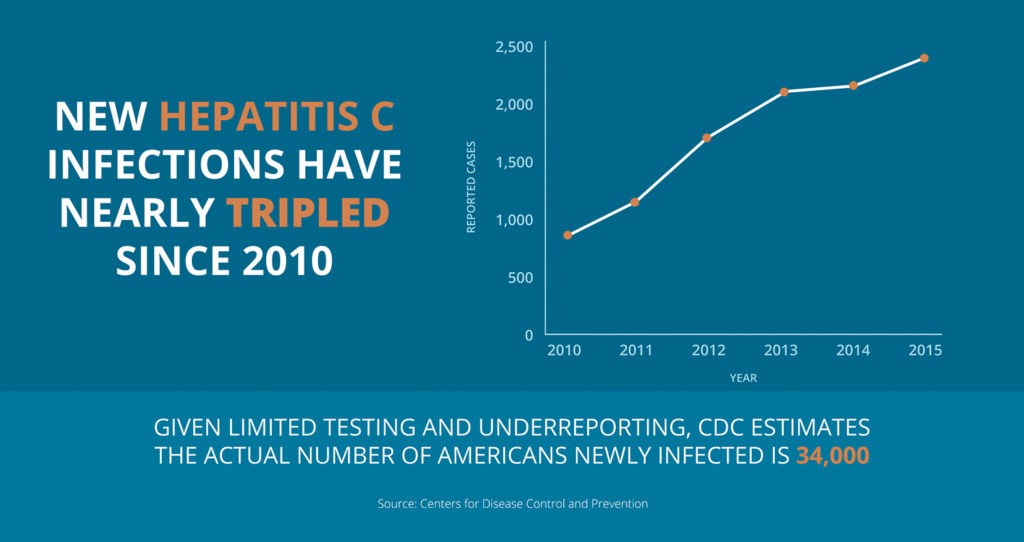
The Reporting Gap
Hepatitis A gets the lion share of headlines because it frequently involves food, which is regulated here in the United States and subject to testing. However, it is hepatitis C that may be most problematic. The hepatitis C virus is transmitted through contact with blood of an infected person, commonly through the use of shared needles in drug usage. It is prevalent among the very poor, homeless, or drug addicted persons. It is estimated that 67% of people who inject drugs have been infected with the virus. Most people with the hepatitis C virus do not even know it. Many whom are infected do not have access to or refuse to seek medical care. Because of this, it is far more difficult to accurately estimate the number of those infected. It is also more difficult to treat current cases, or prevent future ones.
The Lasting Impact
According to the World Health Organization, 19 million hepatitis related deaths are anticipated from 2015 to 2030, absent additional efforts. Prevention efforts can reduce the number of additional infections, though the number of those already infected would remain significantly high for a generation. Among the global health community there is a growing consensus that Hepatitis C could be eliminated in the not too distant future. A recent report from the O’Neil Institute for National and Global Health Law at Georgetown University highlighted this and concludes that the key elements needed for achieving elimination of HCV is adequate surveillance and monitoring, yet the barrier of a population resistant to seeking care remains. Acknowledging a constrained federal budget, the report also highlighted how a relatively modest investment could have a huge impact in furthering the efforts though better utilizing the data already available. These efforts, they say, would lead to such benefits as a plummet in liver cancer rates which in 2010 was responsible for 23,000 liver cancer deaths, as well as save nearly $300 million annually in health care costs avoiding liver transplant surgeries caused by HCV.
What legacy we leave concerning hepatitis will be played out for generations. The effort we put in now could mean eradicating it in the not too distant future.