It Hurts Right Here!

Understanding Sacroiliac Joint Pain and Exploring the Latest Treatment Option Dr. Constantine Fotopoulos of Dickson-Diveley Orthopaedics
A leading interventional physiatrist gives us a glimpse into the world of the sacroiliac joint and what could possibly be a secret cause of low back pain.
Story by Ann Butenas | Sponsored Content
At some point in your life, you are probably going to have to ask the universal question: what is causing this pain in my back? Back pain is a common reason for absence from work and for seeking medical treatment. Not only can it be chronically uncomfortable, but it can also become quite debilitating. Back pain can result from myriad causes, such as age, injury, activity and certain medical conditions.

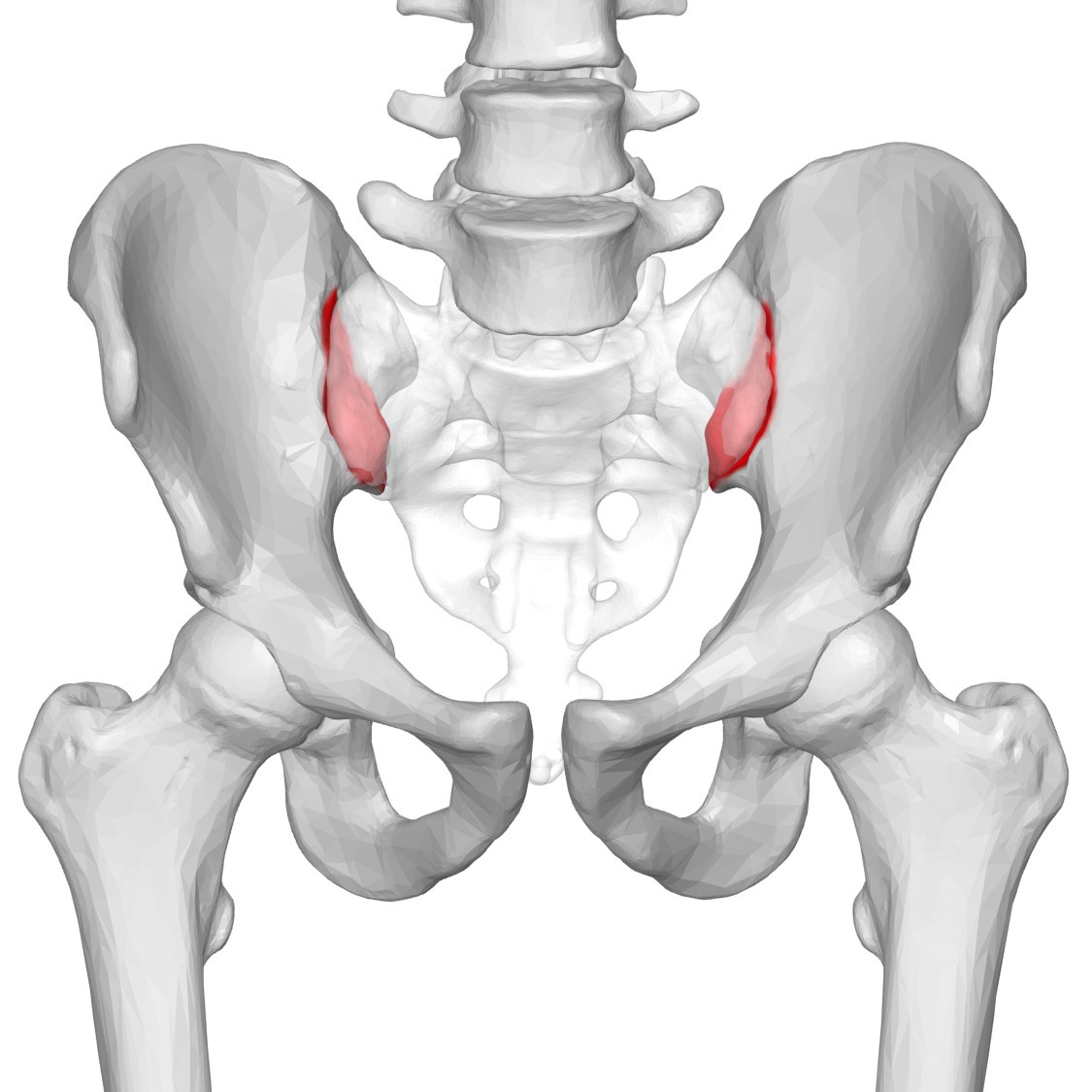
If you stand up from your chair and feel a pain in your lower back, it could be from your sacroiliac joint (SI joint) acting up. There are two of these joints in your body, sitting on each side of your spine, which serve to link your pelvis and your lower spine. They consist of the sacrum, which is the bony part just above your tailbone and right beneath your lower vertebrae, and the top part of your pelvis. Their primary job is to carry the weight of your upper body when you stand or walk and shift that load to your legs. When experiencing SI joint pain, it can present as either dull or sharp. While it starts at the SI joint, it can target the buttocks, groin, thighs and even upper back. It can be triggered simply by standing up, and often you may just feel it on just one side of your lower back.
Inflammation at the joint can occur as a result of playing sports, falling down, or even running regularly. Perhaps one of your legs is longer than the other, forcing you to take uneven strides. Sometimes the pain flares up when the ligaments securing your SI joint together are damaged, causing the joint to move abnormally.
Another contributing factor is arthritis. Ankylosing spondylitis is a type of arthritis that affects the spine and can ultimately damage the SI joint. Pain at this area can also be the result of wear and tear as you age. Additionally, pregnancy can contribute to the pain. During pregnancy, hormones are released throughout a woman’s body that can cause joints to loosen up and move more. This can lead to changes in the way those joints function and move.
Discovering the reason behind the back pain is one thing; determining the best treatment approach is yet another.
Is it time to call the doctor? Finding relief for SI joint pain.
A graduate of the University of Missouri- Kansas City School of Medicine, Dr. Constantine Fotopoulos is board-certified in physical medicine and rehabilitation, pain medicine, sports medicine and undersea hyperbaric medicine. A physician at Dickson-Diveley Orthopaedics, with locations in Leawood and in Kansas City at Saint Luke’s Hospital Campus Medical Plaza, Dr. Fotopoulos specializes in spine and sports medicine. A skilled, respected, experienced and in-demand interventional physiatrist, Dr. Fotopoulos stands among an elite group of orthopedic physicians whose contribution to the field of orthopedic medicine involves personalized care across all subspecialties in orthopedic medicine using state-of-the-art technologies coupled with the best in patient care. Treating SI joint pain is one of the many services he offers.
Choosing the least invasive approach is always preferable when treating SI joint pain. This can include physical therapy exercises designed to improve strength and flexibility. Other treatments may include hot and cold packs, massage, non-habit forming medication and even chiropractic care. Sometimes a steroid injection may be recommended to mitigate the inflammation within the joint.
Dr. Fotopoulos is leading the way in the metro area with a new approach to treating SI joint pain via the LinQ™ – SI Joint Stabilization System by PainTEQ™. However, he relies on a systematic approach to treating the pain based on the individual patient’s response to what he prescribes before turning to this minimally-invasive and highly innovative approach.

It’s important to understand the pain.
“SI joint pain is difficult to diagnose and hard to understand,” revealed Dr. Fotopoulos. “Some individuals have had the pain for years and never really knew what it was. When they get the diagnosis of SI joint pain, it can be bittersweet, as now they can give a name to a pain that otherwise has been difficult to treat. Is this new procedure the panacea or holy grail for SI joint pain? No, and it is also not the only thing available to reduce the pain.”
There is not one physical test that tells you it is SI joint dysfunction, but there are tests a practitioner does to see if it potentially could be. Most important, though, it requires the use of an open and compassionate ear lent directly to the patient.
“My job is to listen to the patient, find out what his or her history is, what hurts, and what makes that person feel better,” expressed Dr. Fotopoulos. “With such a multi-faceted diagnosis, it is hard to treat, and the associated pain can be subtle or glaring. Sciatica pain may even present with it. We call it the Great Pretender, as it can look like anything and is more common than I give it credit for. In some patients, it is present no matter what you treat. In others, it gets better when you treat disc pain.”
Who may be a candidate for SI fusion?
Dr. Fotopoulos indicated potential patients for SI joint fusion may fall into one of several categories.
“The most common patient experiencing this pain is the post-partum individual,” he indicated. “During pregnancy, the pelvis and birth canal are loosened so the ligaments don’t always tighten up as they should after delivery.”
Other causes of SI joint pain may occur as a result of trauma, such as a car accident. Further, certain arthritities may be contributing factors, including psoriatic, rheumatoid and ankylosing spondylosis.
“The SI joint is weird in that no one knows exactly how it works,” commented Dr. Fotopoulos. “There are many theories on it, however. Patients who have SI joint issues may experience pain when getting off the toilet, climbing stairs or during sex.”
Using the LinQ™ – SI Joint Stabilization System by PainTEQ™, Dr. Fotopoulos can safely treat patients with SI joint pain in a minimally invasive manner with faster recovery times and with proven effective results. This particular system is intended for SI joint fusion issues that include degenerative sacroiliitis and SI joint disruptions. The procedure combines both fusion and stabilization of the joint in eligible patients who otherwise might not have benefited from previous non-surgical approaches.

How does it work?
Designed for the interventionalist, this percutaneous procedure involves a small, single incision, about one-quarter inch to one-half inch.
“It is performed in a less invasive way than traditional sacroiliac fusions, which drilled laterally across the pelvis and into the sacroiliac joint into which three pegs were then placed,” explained Dr. Fotopoulos.
Essentially, the LinQ™ SI Joint Stabilization system allows for a single LinQ™ allograft to be placed into the SI joint. This helps patients almost immediately regain joint stability. Since it is not a complete fusion, it creates an environment conducive to long-term fusion.

The recommended treatment plan for SI joint pain.
While surgery is rarely used to treat SI joint pain, there are a few options that can minimize the pain.
“Usually, our treatment plan starts with good physical therapy, which is without a doubt the best treatment,” emphasized Dr. Fotopoulos. “The SI joint is not always well understood by most physical therapists, but there are some who do understand it and can offer the best exercises.”
If physical therapy fails to provide relief, Dr. Fotopoulos has some patients wear an SI joint belt.
“This is worn around the hips, holding the joint in place so it doesn’t move, which helps to reduce the pain,” stated Dr. Fotopoulos. “These are usually worn for about six to eight months.”
Steroid injections are also a way to reduce inflammation. If that fails to deliver pain relief, Dr. Fotopoulos may turn to yet another interventional pain management technique that may also work, such as radiofrequency ablation, for example, which temporarily keeps the nerves from sending pain signals. Electrical stimulation may also be used to stimulate the nerves and muscle tissue surrounding the SI joints.
“If none of these approaches or treatment methods work, then we can consider this new SI joint fusion approach,” said Dr. Fotopoulos. “It is a quick and easy out-patient procedure typically done under local anesthetic with some sedation to help the patient relax.”
Some patients may notice relief immediately after the procedure. Dr. Fotopoulos suggests a restriction of activity for the first two weeks, however.
The bottom line!
“Back pain most often is multifactoral,” Dr. Fotopoulos explained. “Rarely is X the problem and Y is the pain-free solution. We can take away a large portion of the pain with this procedure, however.”
Dr. Fotopoulos can not guarantee any patient will become or will remain pain-free, and they may have to at least take some sort of pain medication to go about the day.
“Could this make a patient pain-free? Sure, but sometimes there still may be some pain. It will just be more tolerable,” said Dr. Fotopoulos.

Saint Luke’s Hospital Campus Medical Plaza Building 1, Ste 610, 4321 Washington St., KCMO and at 3651 College Blvd, Leawood, KS 66211
913.319.7678 ext 3109 | DD-Clinic.com






