January is Cervical Cancer Awareness Month
Story by Cheri Woodsmall
Megan was a normal 27-year-old. She had met the love of her life, recently moved in with a mutual friend of theirs, and started working at the family business full-time. She had a beautiful dog, Rocco, who was her best friend. Her world was perfect in her eyes.
Then something changed. Less than a year into her relationship with her boyfriend, she noticed that she was having quite a bit of pain in her pelvis. Waking up almost every day in pain, she would get up and take an Advil and usually forget about it by the end of the day. She also started to bleed after intercourse. Telling herself that it was just her periods messing with her or changing as she got older, she waited almost an entire year before going to the doctor. She kept putting off regularly scheduled pap smear because as a young woman in her 20s, she didn’t think SHE NEEDED to go to that one appointment.
Megan finally did go to that appointment. And it was during her exam her doctor said, “Well, I’m sorry this is taking so long, but I’m seeing something here that isn’t right. I am going to run some labs, but also just to be on the safe side, send you to a specialist.”
The results came in a couple of days later and that call from her specialist was one she wouldn’t forget. “I regret to inform you that the test came back positive. There is a tumor in your cervix, and it is cancerous. You have cervical cancer and will need to begin treatment with a gynecological oncologist as soon as possible.”
WHAT IS CERVICAL CANCER?
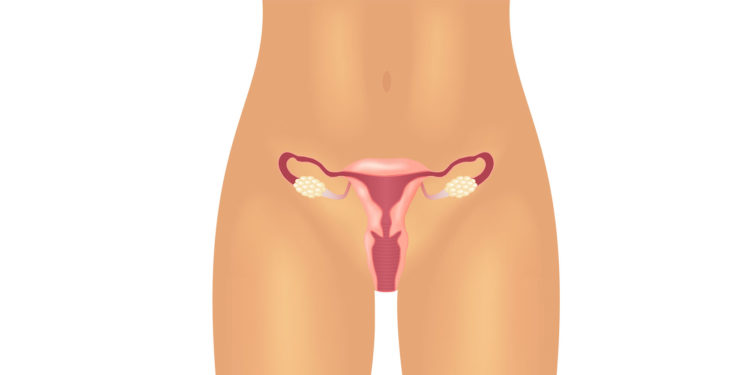
Cervical cancer is cancer that starts in the cells of the cervix. The cervix is the lower, narrow end of the uterus (womb). The cervix connects the uterus to the vagina (birth canal). Cervical cancer usually develops slowly over time. Before cancer appears in the cervix, the cells of the cervix go through changes known as dysplasia, in which abnormal cells begin to appear in the cervical tissue. Over time, if not destroyed or removed, the abnormal cells may become cancer cells and start to grow and spread more deeply into the cervix and to surrounding areas.
TYPES OF CERVICAL CANCER
Cervical cancers are named after the type of cell where the cancer started. The two main types are:
- Squamous cell carcinoma: Most cervical cancers (up to 90%) are squamous cell carcinomas. These cancers develop from cells in the ectocervix.
- Adenocarcinoma: Cervical adenocarcinomas develop in the glandular cells of the endocervix. Clear-cell adenocarcinoma, also called clear-cell carcinoma or mesonephroma, is a rare type of cervical adenocarcinoma.
THE SYMPTOMS OF CERVICAL CANCER
A precancerous lesion of the cervix often does not cause any signs or symptoms. Symptoms or signs do typically appear with early-stage cervical cancer. With advanced cervical cancer, which is cancer that has spread to other parts of the body, the symptoms may be more severe depending on the tissues and organs to which the disease has spread.
Symptoms are changes that you can feel in your body. Signs are changes in something measured, like by taking your blood pressure or doing a lab test. Together, symptoms and signs can help describe a medical problem. The cause of a symptom or sign may also be a medical condition that is not cancer, which is why people need to seek medical care if they have a new symptom or sign that does not go away.
Any of the following could be symptoms or signs of cervical cancer:
- Blood spots or light bleeding between or following periods
- Menstrual bleeding that is longer and heavier than usual
- Bleeding after intercourse, douching, or a pelvic examination
- Increased vaginal discharge
- Pain during sexual intercourse
- Bleeding after menopause
- Unexplained, persistent pelvic and/or back pain
Any of these symptoms should be reported to your doctor. If these symptoms appear, it is important to talk with your doctor about them even if they appear to be symptoms of other, less serious conditions. The earlier precancerous cells or cancer in the cervix is found and treated, the better the chance that the cancer can be prevented or cured.
CAUSES AND RISK FACTORS
All women are at risk for cervical cancer. It occurs most often in women over age 30. Long-lasting infection with certain types of human papillomavirus (HPV) is the main cause of cervical cancer. Most HPV infections go away on their own as the immune system controls the infection. When a high-risk HPV infection lasts for many years, it can lead to changes in the cervical cells that, if untreated, can become cancer.
Some risk factors make it more likely for a person who has a high-risk HPV infection of the cervix to have a persistent infection that leads to severe cervical cell changes that can develop into cervical cancer. These risk factors include:
- Having a weakened immune system: This can lower the body’s ability to fight HPV infection and other diseases. You may be immunocompromised if you:
- Have HIV infection or another disease that weakens the immune system.
- Take medicine to suppress your immune response, such as to prevent organ rejection after a transplant, to treat an autoimmune disease, or to treat cancer.
- Smoking or breathing in secondhand smoke: Those who either smoke or breathe in secondhand smoke have an increased risk of developing cervical cancer. The risk increases the more a person smokes per day and the longer a person has smoked.
- Becoming sexually active at an early age: The risk of high-risk HPV infection that is persistent and ultimately leads to cervical cancer is higher in people who become sexually active before age 18 and in those who have had multiple sexual partners.
- Other reproductive factors: Both the use of oral contraceptives (birth control pills) and giving birth to many children have been found to be associated with cervical cancer risk. The reasons for these associations are not well understood.
- DES exposure in the womb: Being exposed to a drug called diethylstilbestrol(DES) in the womb is an independent risk factor for a type of cervical cancer called clear cell adenocarcinoma. Between 1940 and 1971, DES was given to some pregnant women in the United States to prevent miscarriage (premature birth of a fetus that cannot survive) and premature labor. Women whose mothers took DES while pregnant have an increased risk of cervical cell abnormalities and of clear cell adenocarcinoma of the vagina and cervix.
SCREENING FOR CERVICAL CANCER
The goal of screening for cervical cancer is to find precancerous cervical cell changes when treatment can prevent cervical cancer from developing. Sometimes, cancer is found during cervical screening and is usually easier to treat in the early stages. By the time symptoms appear, cervical cancer may have begun to spread, making treatment more difficult.
There are three main ways to screen for cervical cancer:
- The human papillomavirus(HPV) test checks cells for infection with high-risk HPV types that can cause cervical cancer.
- The Pap test (also called a Pap smear or cervical cytology) collects cervical cells so they can be checked for changes caused by HPV that may—if left untreated—turn into cervical cancer.
- The HPV/Pap co-test uses an HPV test and Pap test together to check for both high-risk HPV and cervical cell changes.
DIAGNOSIS AND STAGING
The following procedures are used to diagnose cervical cancer:
COLPOSCOPY
Colposcopy is a procedure in which the health care provider inserts a speculum to gently open the vagina and view the cervix. A colposcopy usually includes a biopsy.
CERVICAL BIOPSY
Biopsy is a procedure in which a sample of tissue is removed from the cervix so that a pathologist can view it under a microscope to check for signs of cancer. The following types of biopsies are used to check for cervical cancer:
- Punch biopsy is a procedure in which a small, round piece of tissue is removed using a sharp, hollow circular instrument. This procedure is usually done in the doctor’s office.
- Endocervical curettage is a procedure to collect cells or tissue from the cervical canal using a curette (spoon-shaped instrument).
- Loop electrosurgical excision procedure (LEEP) uses a thin wire loop, through which an electrical current is passed, to remove tissue from the cervix. This procedure is typically done in a doctor’s office. It usually takes only a few minutes, and local anesthesia is used to numb the area.
- Cone biopsy is surgery to remove a larger, cone-shaped piece of tissue from the cervix and cervical canal and is done at the hospital under general anesthesia.
Talk with your health care provider to learn what to expect during and after your biopsy procedure. Some people have bleeding and/or discharge after a biopsy. Others have pain that feels like cramps during menstruation.
STAGING CERVICAL CANCER
A cancer stage describes the extent of cancer in the body, especially whether the cancer has spread from where it first formed to other parts of the body. It is important to know the stage of cervical cancer to plan the best treatment. The International Federation of Gynecology and Obstetrics staging system is used for cervical cancer.
Stage 1: Cervical cancer has formed and is found in the cervix only.
Stage 2: Cervical cancer has spread to the upper two-thirds of the vagina or to the tissue around the uterus.
Stage 3: Cervical cancer has spread to the lower third of the vagina and/or to the pelvic wall, and/or has caused kidney problems, and/or involves lymph nodes.
Stage 4: Cervical cancer has spread beyond the pelvis or has spread to the lining of the bladder or rectum or has spread to other parts of the body.
TREATMENT
Your oncologist will work with you to develop the best treatment plan, which may include more than one treatment. Your treatment plan will include information about your cancer, the goals of treatment, the treatment options, possible side effects, and the expected length of treatment.
Treatments can include:
- Surgery
- Cold knife conization
- Sentinel lymph node biopsy
- Hysterectomy
- Radical trachelectomy
- Bilateral salpingo-oophorectomy
- Total pelvic exenteration
- Internal and External Radiation Therapy
- Chemotherapy
- Targeted therapy
- Clinical trials
In Megan’s case, her treatment plan included 5 weekly chemotherapy sessions, daily radiation, 5 internal radiation treatments (requiring surgical placement), and an additional 12 weeks of chemotherapy.
COPING WITH CERVICAL CANCER
A diagnosis of cervical cancer can leave you and your loved ones feeling uncertain, anxious, and overwhelmed. There are important treatment decisions to make, emotional concerns to manage, and insurance and financial paperwork to organize, among other practical concerns.
It is helpful to keep in mind that there are many sources of information and support for people coping with cervical cancer. By learning about this diagnosis and its treatment options, communicating with your healthcare team, and surrounding yourself with a support network, you will be better able to manage your cervical cancer and experience a better quality of life.
The American Cancer Society’s estimates for cervical cancer in the United States for 2022 are:
- About 14,100 new cases of invasive cervical cancer will be diagnosed.
- About 4,280 women will die from cervical cancer.
- 5-year survival rate 66.7%





