Radiofrequency Ablation
A Potential Answer for Chronic Low Back Pain, Knee Pain and Even Certain Types of Headaches
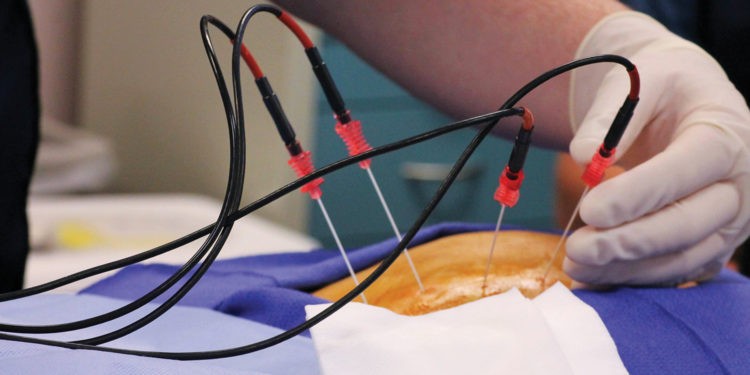
Through the use of radio waves, a small insulated needle is heated up and used to burn the nerves responsible for the pain, and the end resulting is certainly making waves.
It’s no secret that many people live with chronic pain on a daily basis, and while there may not often be cures or specialized treatments for every single issue, there are certain technologies available at this time that are delivering some highly promising results in terms of relief for chronic low back pain, knee pain and certain types of headaches. The medical experts at Dickson-Diveley Midwest Orthopaedic Clinic often turn to a highly-favorable procedure known as radiofrequency ablation in an effort to greatly minimize or, in some cases, eliminate the pain altogether, for patients presenting with these issues.
“Through the use of radiofrequency ablation, we use heat produced by radio waves to cauterize sensory nerves in the body,” explained C. Lan Fotopoulos, M.D., noted interventional physiatrist at Dickson-Diveley. “In addition to treating low back pain, neck pain and headaches, this type of procedure has also been used for tumors as well as for certain cardiac issues.”
In the pain world, when discussing chronic back and neck pain, physicians refer to the facet joints, which are located in the back of the spine. These are the joints that make your back flexible and allow you to bend and twist. Just like other joints, they have a capsule around them, cartilage, and fluid. They are also susceptible to arthritis. A healthy facet joint enables the vertebrae to move smoothly against each other without grinding. Facet joint syndrome results when there is pain at the joint between two vertebrae in the spine. This is also known as osteoarthritis. When these joints become swollen and painful, it is called facet joint syndrome.
The diagnosis of facet joint syndrome is a history-based exam. Simultaneous to ruling out fractures and herniated discs, a physical examination and complete patient history is also taken.
Prior to the actual procedure of radiofrequency ablation, the patient will undergo a medial branch block under local anesthesia through an injection into the medial branch nerve to determine how he or she will respond and if said patient fits the diagnosis of facet mediated pain. If the lower back pain is reduced for a temporary amount of time, then sometimes a second block is done. If the patient responds favorably at that point, then typically a follow-up visit for the radiofrequency ablation procedure is scheduled.
Done on an out-patient basis under x-ray guidance and through the use of light anesthesia, a needle is placed on the medial branch at a temperature of 60-80 degrees Celsius, allowing the radiofrequency waves to cauterize the nerves. The treatment itself usually only takes 15-30 minutes to perform.
Dr. Fotopoulos cautioned, however, that pain relief is not always immediate.
“It can take two to three weeks for the patient to notice the difference,” he stated. “However, the results can last up to 18 months.”
In many cases, when a patient presents with low back pain, a standard treatment option is to treat it with a steroid injection every three to four months, which not only takes additional time out of the patient’s schedule but can sometimes also comes with certain unfavorable side effects.
“With radiofrequency ablation, however, a patient can realize anywhere from six to 18 months – and, in some cases, even permanent results,” explained Dr. Fotopoulos.
With the exception of the brain and spinal cord, all nerves in the body have the potential to regrow. Therefore, additional procedures may be necessary down the road in an effort to manage and control the pain.
In addition to using radiofrequency ablation to treat chronic low back pain and some headaches (such as cluster headaches or those originating from the cervical spine), the medical community has realized within the past few years that this procedure can affect sensation around the knee.
“For example, if you had a total knee replacement but still have knee pain on the geniculate nerve, this procedure can reduce that pain,” said Dr. Fotopoulos. “However, it is advisable for the patient to wait at least year after surgery, and if there is still significant pain but no problem with the prosthesis, then radiofrequency ablation can then be considered a good option at that point.”
Up until a few years ago, chronic knee pain after a total knee replacement, despite a well-functioning prosthesis, was simply met with no viable means of relief, short of physical therapy or certain oral medications.
“While radiofrequency ablation is not 100% guaranteed, a fair number of patients do realize significant reduction in their pain levels,” stated Dr. Fotopoulos. “For those who do not, there are other procedures available, such as dorsal root ganglion stimulation.”




