The Importance of Inclusive Access to Healthcare

Story by Dr. Iman Williams Christians, Director of Grief Programs, Kansas City Hospice & Palliative Care
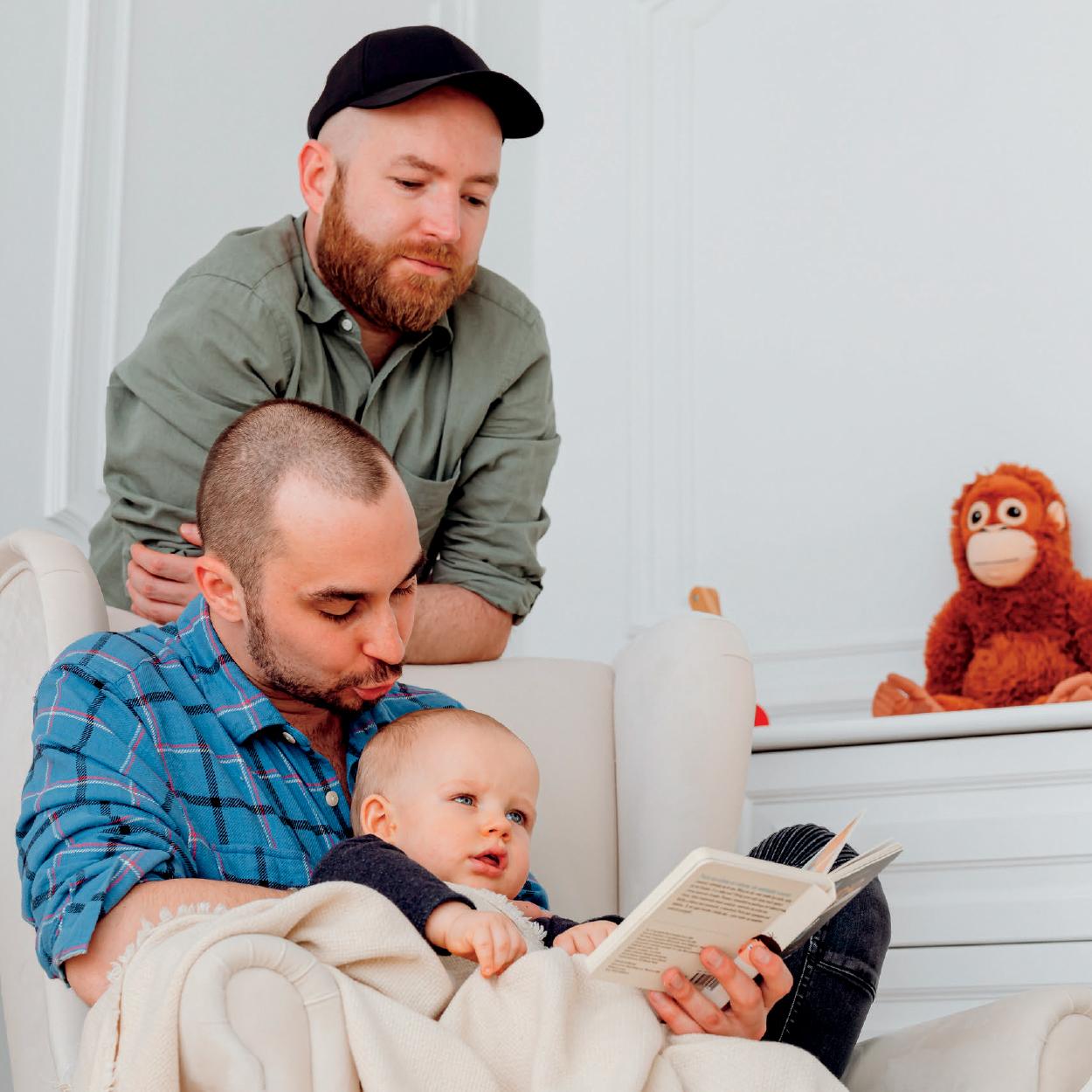
Ensuring access for everyone is important across all areas of healthcare, including people facing serious illness and end-of-life decisions. Physical barriers may be the first thing that comes to mind. It is, of course, important to ensure access regardless of language, vision, hearing, and mobility. But – keep going! Inclusion involves removing many types of barriers to marginalized communities.
That might seem obvious to many people, but in 2018 the American Association of Retired Persons (AARP) found that 57% of the LGBTQ+ community is concerned about healthcare providers not being sensitive to their needs as they age. Defined, LGBTQA+ is an abbreviation for lesbian, gay, bisexual, transgender, queer or questioning, asexual, and more. In fact, one out of ten LGBTQ+ patients have been denied healthcare or provided inferior care and 15% fear receiving health services outside the LGBTQ+ community.
In case one might think the fear is unfounded, according to a 2020 survey of care providers by Gary L. Stein of Yeshiva University:
- 53% thought that lesbian, gay, or bisexual patients were more likely than non-LGBTQ+ patients to experience discrimination at their institution
- 23% actually observed discriminatory care
- 64% said transgender patients were more likely than non-transgender patients to experience discrimination
- 21% observed discrimination to transgender patients
- 14% observed the partner or surrogate of an LGBTQ+ patient being treated disrespectfully
Do these numbers seem significant? They should, considering there’s an increase expected in self-identified LGBTQ+ adults, age 65 and older, from 1.5 million to 3 million, by the year 2030. Some of the barriers to care, specifically palliative and hospice care, include perceptual barriers like:
- I will be refused care because of my gender identity, gender expression, or sexual orientation
- I’ll run the risk of being “outed” to my family members
- I will have to spend my limited time and energy educating my healthcare providers
Other barriers include financial concerns, including transgender patients who may worry about losing coverage for their hormones. In addition, institutions may unintentionally erect barriers including discriminatory admission and employment policies; non-inclusive marketing and outreach materials; and inadequate orientation and training for staff and volunteers.

Steps to Help Ensure Inclusive Access
It can be easier than one might think to help ensure inclusive access, especially at the end of life. First, get to know the patient. Ask questions to ensure you understand your role in the patient’s care. Here are examples of questions that can help you have a clearer picture of the patient’s story:
- What name do you use?
- What sex were you assigned at birth?
- What gender do you identify with as of now?
- What gender pronouns do you use? (e.g., he/him, she/her, they/them)
- What prompted your decision to seek palliative care or hospice care?
- Who do you consider to be your family?
- To whom do you turn for support?
- What information, if any, would you like me to share regarding your illness?
As with all people, advance planning saves much confusion and heartache. Discuss with the patient who will manage their care if they’re incapable of making decisions autonomously. Never assume words like “spouse,” “husband,” or “wife” are formalized legally. Ensure that the patient knows conflict over funeral arrangements can be avoided with a funeral directive. And finally, ensure the patient knows property ownership including land, houses, jewelry, and even photos could be passed to another family member if a significant other is not named in a will.

Easing the Process
It’s easy to make your institution more inclusive from the very start.
Areas to look at closely include:
- Ensuring you have a strong, prominently displayed nondiscrimination statement. Use it on your marketing materials.
- Be sure there’s parity in benefits offered for employees with spouses of different sexes and the same sexes. Take a look at your leadership team. Are there LGBTQ+ individuals in leadership positions?
- Audit your training and orientation. Does new employee orientation include training about specific ways LGBTQ+ people and other underserved populations experience discrimination in healthcare and how to prevent it?
- Make sure your intake forms and processes use language that’s inclusive and not offensive.
It’s easy to see the many ways LGBTQ+ members of society could be marginalized when it comes to healthcare. The good news is, it’s even easier to take small steps at your organization to ensure access to healthcare and equal treatment are available to everyone.
Visit Kansas City Hospice & Palliative Care at KCHospice.org.






