Breath Easier
November is National COPD Awareness Month
Story by Cheri Woodsmall
“I was on a bicycle ride with some friends and my shortness of breath got so bad that I had to stop and rest for a good period of time. And my friends all became really concerned about me being able to continue riding that day. I decided it was time to go to see my doctor. I explained how it had felt like somebody was sitting on my chest, and I couldn’t breathe in deeply, and I couldn’t catch my breath and that I was feeling lightheaded at some point because I just felt I was winded when I wasn’t doing anything.”
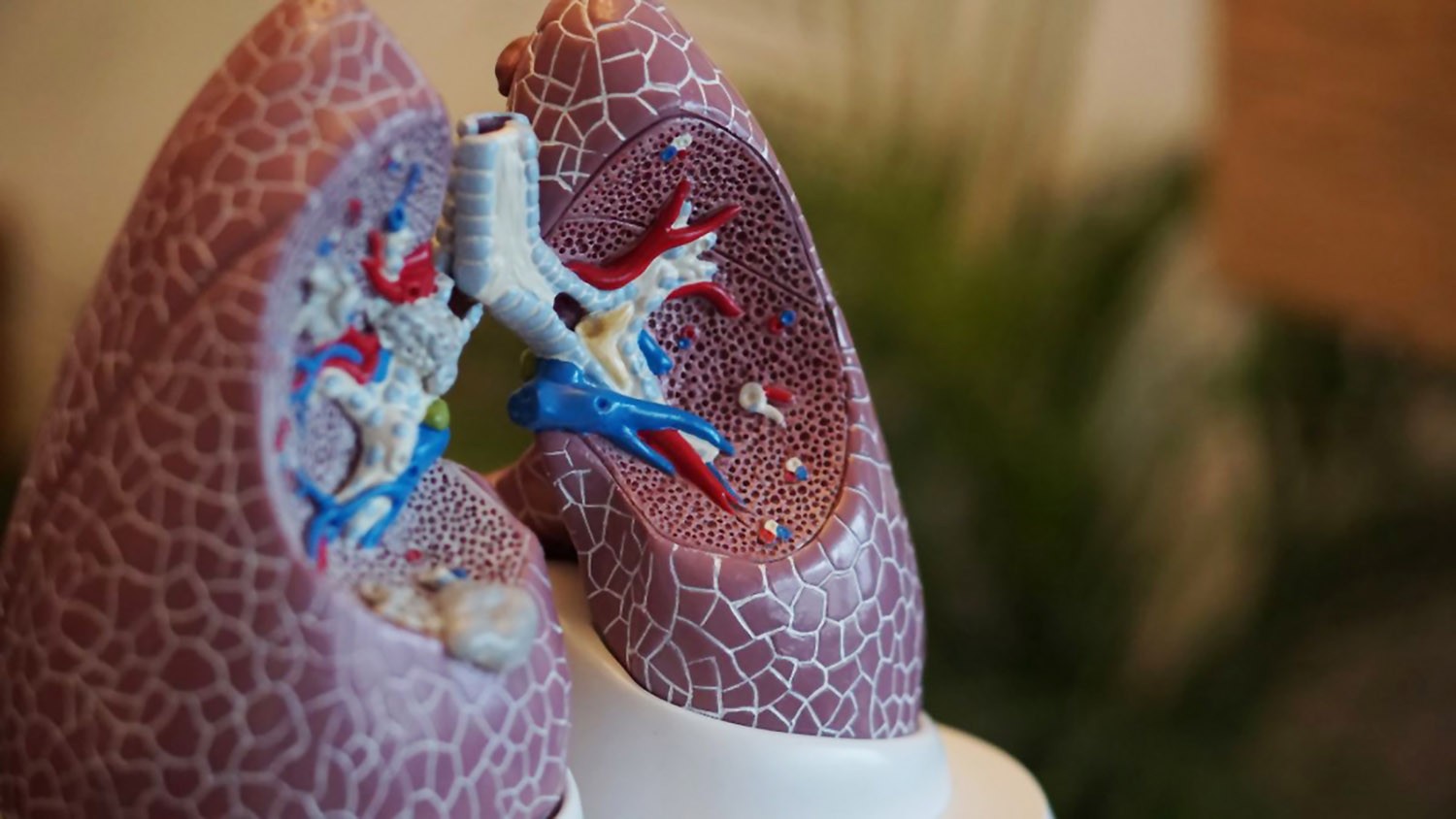
This is just one of the stories of the more than 12 million people in the United States that are known to have the advanced lung disease chronic obstructive pulmonary disease (COPD). Experts believe that many more may not be diagnosed. This common condition, the fourth leading cause of death in the US, inhibits the flow of air into and out of the lungs, making it harder to breathe over time.
The American Lung Association reports that COPD is the fourth leading cause of death in the United States, but as a chronic, progressive disease, most patients will live with the disease for many years.
COPD cannot be reversed, and there is currently no cure. However, with early detection, proper treatment, and some lifestyle changes, patients can slow its progression and breathe their best. For National COPD Awareness Month this November, learn more about this disease, signs to watch out for, and the number-one thing that patients can do to better manage their condition.

COPD CAUSES AND EFFECTS
The #1 cause of COPD is smoking. Tobacco smoke brings toxins and harmful particles into the lungs; over time, they cause permanent damage to the lung tissue. However, other outside factors can also lead to COPD, such as exposure to secondhand smoke, unclean air, or dust and fumes. COPD can also be generated from inside the body, from causes such as the effects of frequent asthma flare-ups and very rare genetic conditions.
The damage caused by COPD comes in multiple forms. The airways leading to the lungs narrow and/or get blocked with mucus. Inside the lungs, air sacs normally take in oxygen and send out carbon dioxide, but in COPD, this tissue breaks down. With less oxygen for fuel, the systems of the body get weaker, including blood circulation and muscle function. Therefore, patients with COPD must work harder to inhale and exhale, and are more prone to feeling tired or short of breath.
SYMPTOMS AND DIAGNOSIS
Many patients are not diagnosed with COPD until the disease is advanced enough that its symptoms are interfering with daily life. Signs to watch for include:
- Shortness of Breath: When you have to work harder to breathe, and find it hard to catch your breath.
- Cough: Coughing can occur any time of the day or night.
- Wheezing: This is a result of air trying to flow through a narrow airway. You may hear a slight whistling or squeaky sound.
- Chest Tightness: The feeling that something heavy is sitting on your chest, restricting your breathing.
Diagnosis of COPD involves testing through a procedure called spirometry. During the test, patients blow air into a mouthpiece attached to a small machine, which calculates the amount and speed of the air blown out. Other procedures that may also be done in order to make a diagnosis include chest X-ray and/or blood testing.
DISEASE TREATMENT AND MANAGEMENT
Although there is no cure for COPD, there are some medical interventions that can help slow progression and reduce symptoms. Medications to aid in breathing, supplemental oxygen, and in some cases surgery may be used to help treat COPD.
However, perhaps the most important actions are those that patients can take in their daily lives, including:
- Quit smoking: For COPD patients who smoke, quitting is almost certainly the biggest improvement they can make. Quitting helps medications work better, boosts heart health and immunity, and drastically decreases the rate of damage to the lungs.
- Seeking quality air: Because lungs have a direct connection to the outside world, it’s important to give them the healthiest possible air. Avoiding secondhand smoke, smog, dust, chemical fumes, high humidity, and extreme temperatures make breathing easier. At home, change furnace filters regularly, or consider an air purifier.
- Healthy diet and activity: Patients who may be overweight, losing weight can lessen pressure on the systems of the body, including the lungs. Underweight patients may need more calorie-rich foods to maintain a healthy weight. Physical exercise can have tremendous benefits; programs such as cardiopulmonary rehabilitation are tailored especially to help patients with chronic heart or lung disease make substantial physical gains.
If left uncontrolled, COPD can escalate until the person has an exacerbation (when symptoms get so severe that emergency care is needed). But with knowledge, appropriate treatment, attention to symptoms, healthy choices, and adequate support from caregivers and clinicians, patients with this disease can minimize their symptoms and stay safe and independent right at home.
MAINTAINING CONTROL OF COPD DURING THE COVID19 PANDEMIC
Managing chronic obstructive pulmonary disease (COPD) is always important, and especially so right now, as individuals living with a chronic lung disease are at a higher risk of severe illness and complications from COVID-19. However, misinformation about COVID-19 has made it hard for people with chronic conditions to determine how to stay safe.
Q: What additional steps should I take to prevent becoming ill with COVID-19?
Because COVID-19 is a new disease in humans, our immune systems haven’t yet developed defenses against it and there’s currently no vaccine. The best way to avoid illness, regardless of age or health status, is avoiding exposure to the virus.
For individuals living with COPD, stringent adherence to the safety precautions is vital. This means staying home as much as possible to avoid potential exposure to the virus. When in public, maintain social distance of at least six feet from people, wear a cloth face covering and encourage others to do the same. Also, wash your hands often and clean, then disinfect frequently touched surfaces.
Q: How can I maintain control of my COPD during the COVID-19 pandemic?
COPD control is especially vital right now in case of exposure to the virus that causes COVID-19. Continue controller medications for COPD to maintain lung health. To limit potential exposure to COVID-19, find out if mail-order pharmacy options are available to you, and if your insurance allows, secure a 90-day supply of prescription medications. Don’t delay important visits or ignore flare-ups or new symptoms. COPD complications can become serious if left untreated. If telemedicine isn’t an option, bear in mind that doctor’s offices have adopted new safety practices during in-person visits.
Q: Should I continue to use my nebulizer at home?
Taking medication correctly is a major component in successfully controlling chronic lung diseases. In certain areas, there have been reported shortages of metered dose inhalers (MDIs) due to increased demand in healthcare settings. Nebulized therapy continues to be a safe, effective way to take inhaled medications at home during the pandemic, though special steps should be taken if you have suspected or confirmed COVID-19.
Q: What additional precautions should I take if I have suspected or confirmed COVID-19?
If you have suspected or confirmed COVID-19, maintain home isolation to protect other household members from potential infection. This includes the following additional safety precautions when using your nebulizer:
- Wash your hands before and after your treatment
- Use your nebulizer in an area that minimizes potential exposure of the aerosolized droplets to other household members. You might consider an outdoor patio or porch, or a room indoors where the air is not recirculated throughout the house and nobody else will enter for 1-2 hours, which is long enough for the droplets to no longer be airborne.
- Clean and disinfect your nebulizer
Your healthcare provider will work with you on when you can discontinue home isolation and resume normal nebulizer use. Contact them at the first sign of a new, severe or concerning respiratory symptom so they can help you come up with a home treatment plan. While most people recover from COVID-19 at home, COPD elevates your risk for severe symptoms. So be sure to seek emergency care for the following symptoms: trouble breathing, pain or pressure in your chest, development of a bluish tinge to your lips or face, and new confusion or inability to wake or stay awake.
Q: Where can I find trusted information?
You can trust the American Lung Association to provide science-based information and resources. Visit Lung.org or call 1-800-LUNGUSA for more information about COPD, COVID-19, nebulized therapy or any other respiratory topic.