Rockhill Orthopaedic Specialists

Advanced Techniques and Emerging Technologies in Orthopaedics
SPONSORED CONTENT
Rockhill Orthopaedics prides itself in always being at the forefront of introducing new technologies to improve patient care. Their innate ability to use advanced techniques and emerging technologies enables them the best means to serve their patients.
Clinical Technologies vs Process Innovations
Emerging clinical technologies, such as Stem cells, PRP-platelet rich plasma, implants and scaffolds all promise enhanced tissue preservation and faster healing. Process innovations are equally important as they utilize new or significantly improved changes in technique, technology and/or use of equipment to improve patient outcomes. Let us explore some advanced techniques and emerging technology that Rockhill Orthopaedic providers are utilizing to help patients recover faster from Carpal Tunnel Surgery, Rotator Cuff Repairs, Complex Regional Back Pain and Lumbar Stenosis.

Fast Track Carpal Tunnel Clinic and Endoscopic Carpal Tunnel Release
Dr. Christopher Maugans is a board certified orthopaedic surgeon with a fellowship in hand and microvascular surgery who has engineered a fast track carpal tunnel clinic at Rockhill Orthopaedics. This new efficient clinical model enables patients to be seen by the physician, have any diagnostic testing completed at the time of service and leave with a proper diagnosis along with all available treatment options for their Carpal Tunnel Symptoms. If Surgery is warranted, Dr. Maugans performs both traditional open surgical release, as well as the specialized endoscopic carpal tunnel release.
Carpal tunnel syndrome is caused by pressure on the median nerve. The carpal tunnel is a narrow passageway surrounded by bones and ligaments on the palm side of your hand. When the median nerve is compressed, the symptoms can include numbness, tingling and weakness in the hand and arm.
Causes of carpal tunnel originate from a combination of factors, including:
• Repetitive Motions of your hands or wrists
• Wrist Trauma or injury
• Female-sex/pregnancy
• Increased Age
• Exposure to Cold
• Working with Vibrating Tools
• Certain Medical Conditions, such as Diabetes, hypothyroidism and Rheumatoid Arthritis
Symptoms of carpal tunnel syndrome may include:
• Numbness, tingling, burning, and pain in the thumb and index, middle, and ring fingers
• Shock-like sensations that radiate to the thumb and index, middle, and ring fingers
• Pain or tingling that may travel up the forearm toward the shoulder
• Weakness and clumsiness in the hand, making it hard to perform fine movements
• Dropping things — due to weakness, numbness, or a loss of proprioception
In most cases, the symptoms of carpal tunnel syndrome begin gradually—without a specific injury. Many patients find that their symptoms come and go at first. However, as the condition worsens, symptoms may occur more frequently or may persist for longer periods of time.
Diagnosis & Treatment Options
Carpal Tunnel Syndrome will worsen over time, for most people without some type of treatment. Dr. Maugans states, it is important to be evaluated and diagnosed by your doctor early on, as it may be possible to slow or stop the progression of the disease.
Non-Surgical Treatments:
• Lifestyle changes. If repetitive motion is causing your symptoms, take activity breaks.
• Exercises. Stretching or strengthening moves can make you feel better.
• Immobilization. Wearing a splint to immobilize your wrist may help by lessening pressure on your nerves, which can help you sleep better.
• Medication. Anti-inflammatory drugs or steroid shots may help to decrease swelling.

Surgical Treatments:
• Open Surgical Release – In open carpal tunnel release surgery, the transverse carpal ligament is cut, releasing the median nerve. The size and shape of the incision may vary, but the incision is usually 2 inches long.
• Endoscopic Carpal Tunnel Release – Endoscopic carpal tunnel surgery uses a thin, specialized device with a camera attached (endoscope), guided through a small incision at the wrist and a smaller incision in the palm (two-portal technique). The device allows usage of both the camera and the cutting tool.
Dr. Maugans states that he “has found throughout his training and clinical practice, patients seem to recover a little faster and have a little less discomfort with a minimally-invasive approach.” However, “both endoscopic and open carpal tunnel release have benefits and risks. The risks and complication rates are typically very low. Despite the faster early rehabilitation attributed to endoscopic surgery, studies do not show that one procedure is better than the other in terms of long-term nerve recovery. Patients do report a 5% better overall satisfaction rate with the Endoscopic Release vs Open, however not every patient is an ideal candidate for endoscopic surgery.”
Call Rockhill Orthopaedic Specialists to schedule an appointment. Be sure to ask for Rockhill Orthopaedic’s new Fast Track Carpal Tunnel Clinic at 816-246-4302.

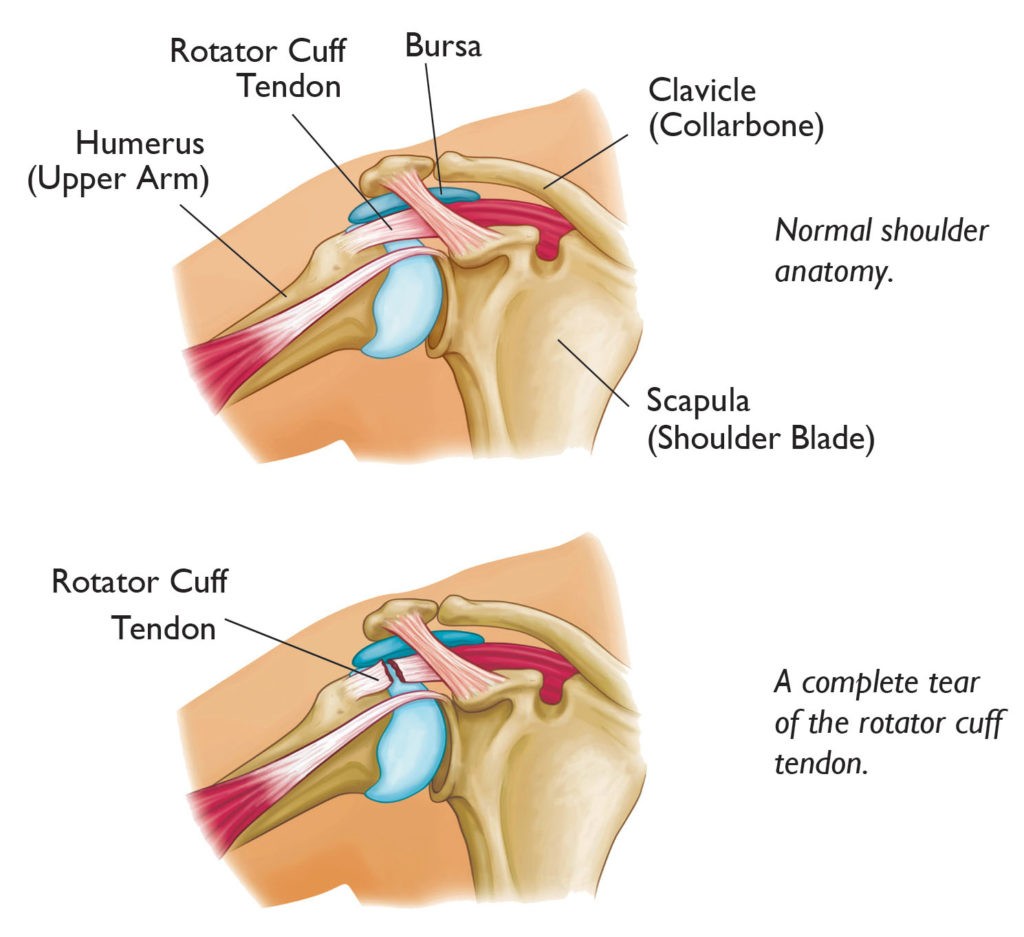
Regeneten Bioinductive Implant
The physicians at Rockhill utilize the latest orthopaedic techniques to help patients achieve the best outcomes. One such technique is the Regeneten Bioinductive Implant, an advanced technology that can be used to repair the rotator cuff of the shoulder. Dr. Wes Frevert is a board certified Orthopaedic Surgeon with a fellowship in sports medicine, who specializes in this advanced surgical technique to repair rotator cuff tears, as it has been shown to improve the healing process with a significantly faster recovery in most cases.
The implant is a collagen scaffold about the size of a postage stamp and is derived from bovine achilles tendons from a secluded herd of cattle in New Zealand. The surgery can be performed with a minimally invasive technique utilizing small incisions to insert and attach the implant. It integrates biologically into the injured tendon to facilitate healing and strengthening.
The Regeneten Bioinductive implant has been extensively tested for safety and has not shown any adverse effects for the patient. In other types of surgical techniques, some implants could cause the body to have an allergic reaction, but this one doesn’t seem to do that.
Dr. Frevert said it can be deployed with standard arthroscopic incisions. “Successful rotator cuff repair requires mechanical stability and biology for successful tendon healing. In conventional rotator cuff repair, anchors and stitches are used to provide mechanical stability. The biologic component relies upon the body’s ability to provide the necessary components through the generation of blood vessels to supply nutrients. Traditionally, this is stimulated with techniques to drill small holes in the bone, but sometimes this is not enough. Emerging “regenerative” technologies such as stem cells and PRP are being utilized is some cases; however, these have failed to demonstrate consistent benefits in clinical studies. The Regeneten scaffold provides biologic support for tendon healing and has demonstrated good results in clinical studies.”

Imagine a rope holding up a weight. Using the implant is like adding supplemental fibers to the existing rope. It’s not adding another rope, but more like wrapping something around the rope that makes it grow stronger.
Tears occur from trauma, stress or general wearing of the tendon over time, and the implant helps with the management and the protection of tendon injuries without a huge loss of tissue. Dr. Frevert has found success in treating both partial and full tears with the implant. “For partial thickness cuff tears, it can be used without any other fixation. Previous treatment of partial thickness tears relied upon mechanical fixation, typically performed by releasing the intact rotator cuff tissue and then fixing it back down along with the torn tissue. The scaffold can be laid down over the intact tissue, allowing the remaining, intact rotator cuff tissue to provide mechanical stability while the scaffold aids the body’s biologic healing which was inadequate in the native tissue.”
Both types of rotator cuff surgery – with and without the implant – can work well in the long run. But the implant may be more effective in allowing people to get back to their lives, sooner.
Dr. Frevert has found, “In cases with partial thickness tears, patients are out of their sling in a few days instead of 6 weeks. For full thickness tears, it can be used to augment conventional repair to improve healing and reduce the risk of recurrent tear by promoting healthier tissue formation. I utilize it for both scenarios. Right now, it is primarily being used in partial thickness tears and revision cases. As more studies are completed, I anticipate that this scaffold (and other similar products that will likely become available) will become standard in most rotator cuff surgery.”
Over time, the implant will become more standard practice and hopefully will become available for everyone who needs it. If the research can prove clinical benefits with cost effectiveness, then more patients will reap the rewards of this surgical technique. The cost-effectiveness factor includes that the surgery may reduce or eliminate the need for revision surgeries, prolonged physical therapy and the patient’s time out of work. This technique has been found to biologically improve healing and new tissues reduce the peak strain at the site of the tear. The body gradually absorbs the patch within 6 months and leaves a layer of new tendon-like tissue to biologically augment the existing tendon. One year after surgery 94% of patients have a high patient satisfaction rate.
Call Rockhill Orthopaedics at 816-246-4302 to learn more about this advanced surgical technique.

Minimally Invasive Treatment for Lumbar Spinal Stenosis
Dr. Jarron Tilghman, a double board certified and fellowship-trained interventional physiatrist at Rockhill Orthopaedic Specialists, is now offering a new and advanced treatment procedure for the management of lumbar spinal stenosis.
The lumbar spine (lower back) consists of five vertebrae in the lower part of the spine, between the ribs and the pelvis. Lumbar spinal stenosis is a narrowing of the spinal canal, compressing the nerves traveling through the lower back into the legs. While it may affect younger patients, due to developmental causes, it is more often a degenerative condition that affects people who are typically age 60 and older.
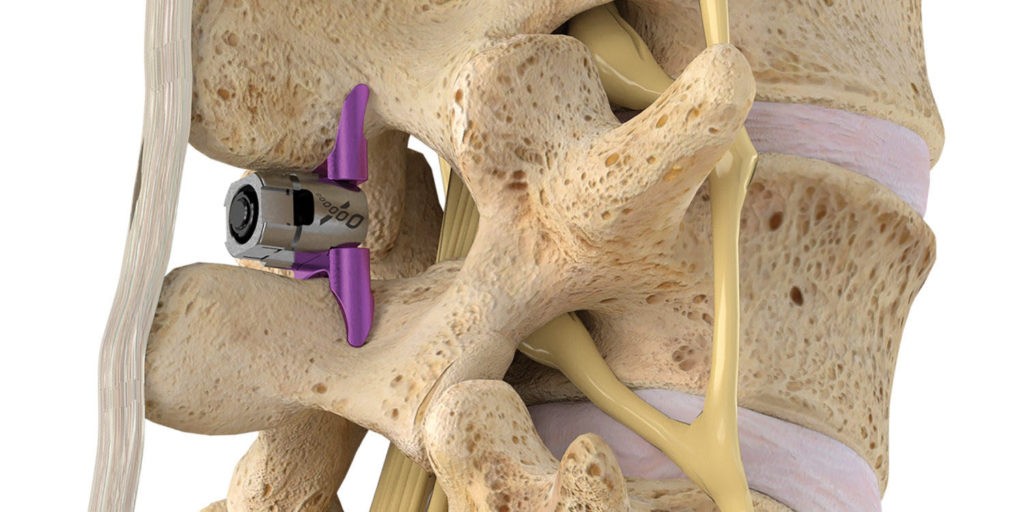
Dr. Tilghman began performing the innovative Vertiflex® procedure, which is an x-ray guided indirect lumbar decompression with the implantation of an interspinous spacer that is placed inside the spine to prevent reduction of the space when standing or walking. This spacer helps to relieve pressure off of the nerves, which in turn alleviates leg and back pain symptoms that often accompany the condition. A recent study revealed decompression with the implantation of an interspinous spacer, can help reduce pain in the low back and legs by as much as 80% and last up to 5 years following the procedure. Dr. Tilghman states “that his patients report dramatic pain relief within 7 days following the procedure.” If you suffer from low back and leg pain which prevents prolonged standing and walking even for short distances, the Vertiflex® procedure may be right for you.
Call (816) 246-4302 to schedule an appointment with Dr. Tilghman.
Study Source: Nunley et al., Clin Inter Aging. (2017)
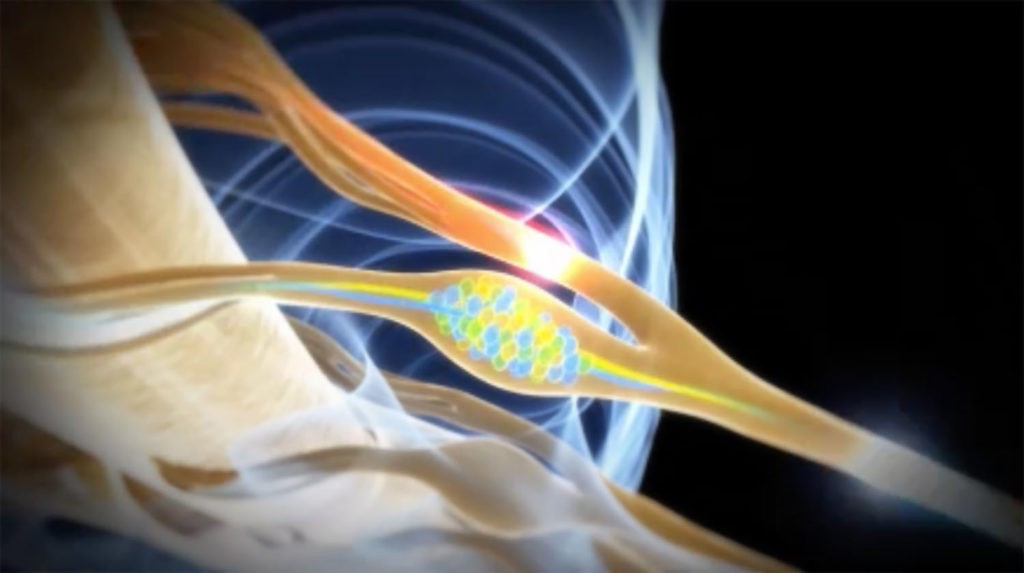
Complex Regional Pain Syndrome Management in the Lower Limb
If you suffer from at least 6 months of persistent pain, swelling, discoloration, and temperature changes in the lower limb following a hernia repair, total hip replacement, total knee replacement, or foot/ankle surgery, Dorsal Root Ganglion Stimulation-DRGS may help you with pain relief. The Dorsal Root Ganglion is a tiny structure which branches from a nerve root and primarily functions to transmit pain signals from the peripheral nervous system into the spinal cord and ultimately to the brain. Dr. Tilghman was specially trained to perform DRGS-in the lower limb following certain surgical procedures, wherein patients suffer from persistent pain. Dorsal Root Ganglion Stimulation (Abbott®) consists of a two-phased approach to provide localized pain relief in specific anatomical regions in the lower limb. Phase 1 (the trial) involves the minimally invasive placement of temporary electrical leads using x-ray guidance in the region of a specific nerve root. The trial typically lasts up to 7 days. If significant reduction of symptoms and improvement in overall functional mobility are achieved, patients are then referred for Phase 2 (permanent implantation). A recent study demonstrated that patients with complex regional pain syndrome in the lower limb had more dramatic pain relief with Dorsal Root Ganglion Stimulation compared to conventional Spinal Cord Stimulation.
Contact our office for a consultation with Dr. Jarron Tilghman to see if this advanced treatment option will help you. (816) 246-4302.
Source: Deer et al., Pain. (2017)







