Vertebroplasty and Sacroplasty

Relieving Back Pain Caused by Compression Fractures
These minimally invasive procedures can be effective in providing pain relief for patients suffering from a spinal fracture.
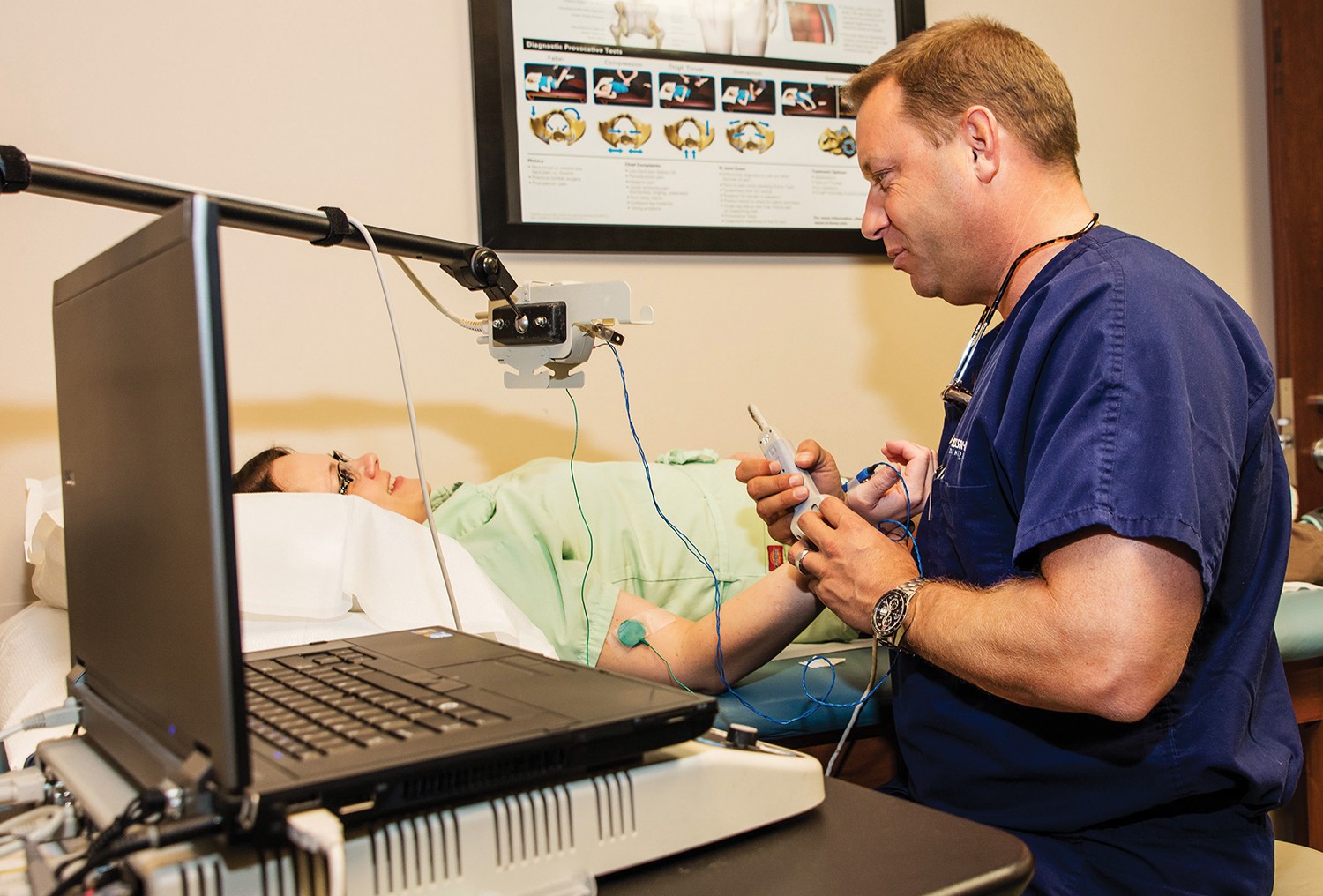
Hippocrates supposedly once noted, “Healing is a matter of time, but it is sometimes also a matter of opportunity.” Meet Dr. C. Lan Fotopoulos, not only an esteemed medical provider but also a provider of opportunity, especially in matters of spinal pain relief.
A graduate of the University of Missouri – Kansas City School of Medicine, Dr. Fotopoulos is board-certified in Physical Medicine and Rehabilitations, Pain Medicine, Sports Medicine and Undersea Hyperbaric Medicine. Additionally, he has worked as an emergency room physician and also served as a lieutenant commander and diving and undersea medical officer in the United States Navy. He is currently practicing medicine at Dickson-Diveley Orthopaedics, with locations in Leawood and in Kansas City at Saint Luke’s Hospital Campus Medical Plaza, where he specializes in spine and sports medicine. His experience and specialized expertise is why patients continually turn to him and his team of experts for the best in patient care, outcomes, and overall satisfaction. Even more specifically, if a spinal compression fracture is keeping you from living a more productive and pain-free life, then Dr. Fotopoulos just might have a resolution for you.

Typically caused by a loss of bone mass, due to osteoporosis, compression fractures can be a part of aging. Anything from a fall to lifting a heavy object or even just coughing may cause a fracture of the back bones. Symptoms related to a compression fracture can include back pain, loss of height and a hunched-forward posture. While standard treatments usually point to physical therapy and/or medication to relieve the pain, there are some minimally-invasive procedures that, for the right candidate, can offer a significant source of pain relief and improved quality of life.
Recognized as a leading expert in the practice of vertebroplasy and sacroplasty, Dr. Fotopoulos offers patients who are candidates for these procedures a relatively simple way to stabilize the spinal fracture and thereby greatly minimize or, in many cases, eliminate the associated pain caused by the fracture.
In a nutshell, vertebroplasty is a minimally invasive surgical procedure done on an out-patient basis typically in 30 minutes under IV sedation wherein a small puncture is made in the patient’s skin (instead of a larger, open incision) through which a biopsy needle is inserted via x-ray guidance. From there, an acrylic bone cement is injected into the fractured vertebra, essentially filling the spaces within the bone. Because the cement hardens quickly, the fragments of the fractured vertebra congeal quickly to stabilize the bone and support the spine.
“Basically, we are creating a cast in the bone,” illustrated Dr. Fotopoulos.

DIAGRAM OF VERTEBROPLASY: Acrylic bone cement injected into a fractured vertebra
Vertebral compression fractures can be caused by osteoporosis, trauma or diseases affecting the bone. Osteoporosis is a skeletal disorder marked by compromised bone strength predisposing a person to an increased risk of fracture. This most commonly occurs in women who are post-menopausal, but it can happen to older men and to people who have used steroid medications over an appreciable amount of time. Trauma factures can incur with a fall from a tall height wherein the person either lands on his or her feet or buttocks. It can also be the result of a car accident. Additionally, these fractures can occur due to pathologic reasons, such as cancer or infection in the bone. Once a fracture has been sustained, it is important to seek medical assistance as quickly as possible for optimal results. For individuals with severe and disabling pain caused by a compression fracture, vertebroplasty has been shown to relieve pain, increase mobility and reduce the use of pain medication.
“If you had a compression fracture forty years ago, you were basically put on bed rest,” noted Dr. Fotopoulos. “At that point, you were already compromised and some people would even die as a result.”
While some conventional treatments for vertebral fractures today include rest, pain relief via nonsteroidal anti-inflammatory drugs, home stretching exercises, and/or applying ice to the injured area (all under the advisement of a physician), verterboplasty can be an effective treatment method for qualified patients.
“The pain relief is relatively immediate for the patient,” emphasized Dr. Fotopoulos.
This procedure is designed to reduce the risk of a new fracture, as statistically, once a person has one such osteoporotic fracture, there exists a five-fold risk of developing a second one within a year.
“If we can get the biomechanics to return to the previous state – back to the same physical geometry – we can then evaluate the patient and treat for osteoporosis through calcium, vitamin D, or medications such as Boniva or Forteo,” explained Dr. Fotopoulos.
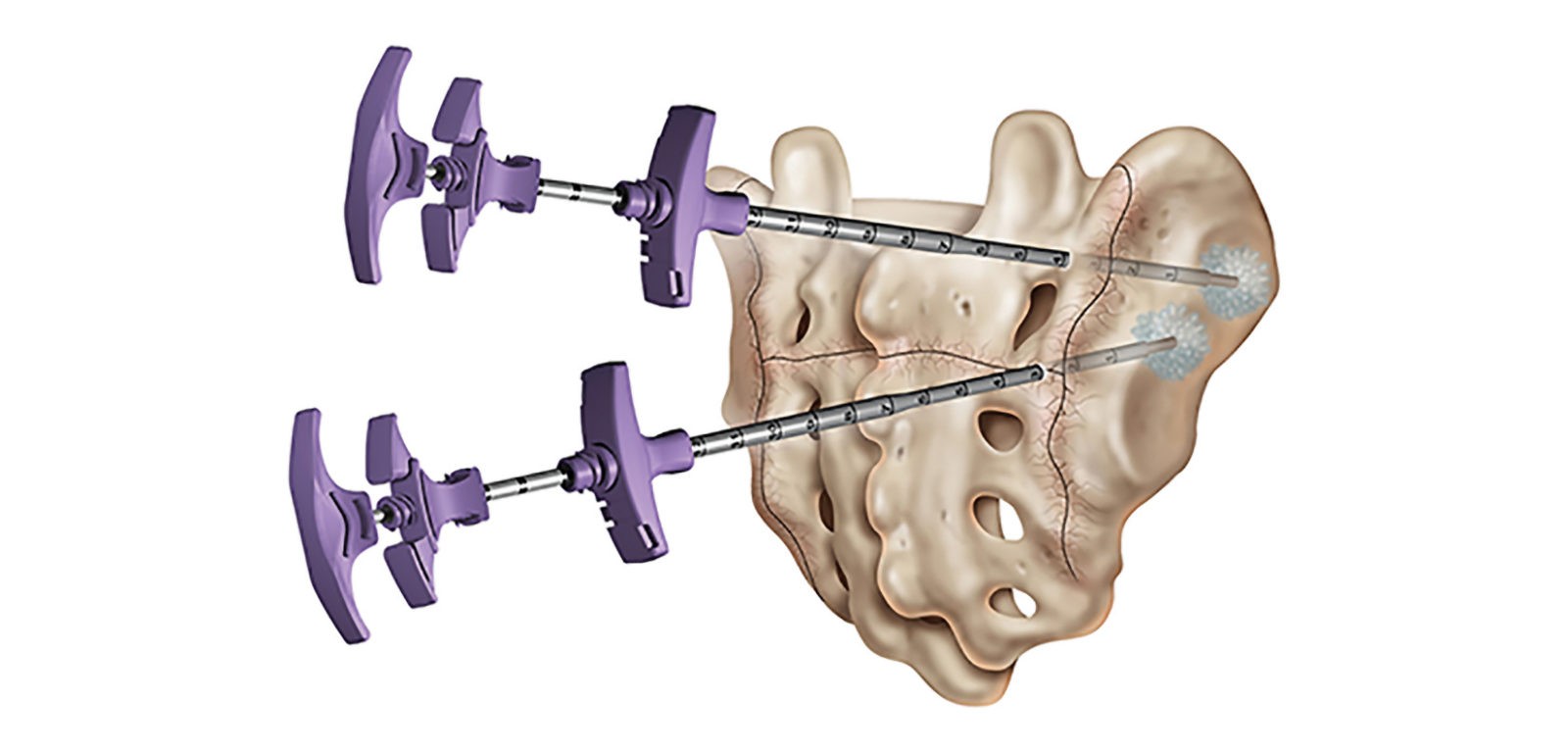
DIAGRAM OF SCAROPLASTY: The cement is injected into the sacrum fracture versus the vertebral body.
Sacral fractures (referring to the tailbone, which is the triangle shaped bone found at the bottom of the spine) are a common source of lower back pain, the typical treatment for which includes appreciable bed rest. However, that comes with complications that result from immobility: deep venous thrombosis, pulmonary embolus, muscle atrophy, decreased cardia function and even psychological changes. The sooner a patient can return to an ambulatory state, the greater the chances of avoiding such complications.
The leading cause of such fractures, again, is osteoporosis, which as indicated more commonly affects elderly women. Other causes may include radiation exposure, arthritis and chronic steroid use. The chief complaint among patients with sacral insufficiencies is lower back pain, primarily acute in nature, and most notably associated with minimal trauma. As a result, such non-specific symptoms, partnered with imaging findings, may make a diagnosis difficult and even unrecognized. Therefore, for a fracture of the sacrum, it is necessary to acquire a high degree of acuity to detect one and accurately diagnose the fracture.
“MRIs are frequently done, but those don’t include the tailbone most times,” Dr. Fotopoulos indicated. “Therefore, nothing may show on it, but as time goes on, someone astute enough may order an MRI specifically of the tailbone and that would be a way to diagnose a sacral fracture. A sacral fracture can present for a very long time but not be treated, as there has not been an accepted treatment option for them. However, I have treated them for 10 years now through a procedure called sacroplasty, which is now Medicare-approved.”
Referred to as a variant of vertebroplasty, scaroplasty is a minimally-invasive percutaneous procedure that can be noted as an alternative approach to conventional treatments and therapies. While it is similar to vertebroplasty, the cement is injected into the sacrum and the sacrum fracture instead of into the vertebral body. It is performed as a means to reduce pain and improve stability.
Dr. Fotopoulos explained that through sacroplasty, a large bore needle is placed into the sacrum and cement is applied to the fractured bone shards. Performed in a specialty hospital, like those used by Dr. Fotopoulos, this same day procedure takes approximately 30 minutes to complete, and most patients will have almost immediate results.
Unique to a sacral fracture, noted Dr. Fotopoulos, is that most of the time people can recall the incident but do not realize how insignificant the injury was.
“Perhaps you felt a pop when reaching for something on a high shelf or when you bent forward or sat down in a chair,” explained Dr. Fotopoulos. “More specifically for people who have vertebral compression factures there is pain that cannot be relieved, and they have tried everything. The doctor may do an x-ray and make a diagnosis, but it could be old healed factures from years ago, and you can’t treat older ones.”
For younger patients, treatment of a sacral fracture usually involves a brace and the use of a doughnut upon which to sit, but for the older population, braces tend to be relatively uncomfortable, so compliance in using them may be minimal or even non-existent. If the patient does not wear the brace, there is no benefit. Therefore, per Dr. Fotopoulos, the appropriate treatment is sacral augmentation.
The long-term prognosis for vertebral and sacral augmentations are usually quite good, but if the patient is osteoporotic, additional measures must be met.
“I always have the patient come back for a two-week follow-up after the procedure,” expressed Dr. Fotopoulos. “I then get them on a board with a specialist on bone health, with an internal medicine doctor, with an endocrinologist and/or with a nurse practitioner who focuses on bone health for appropriate bone density evaluation to treat the osteoporosis initially or to optimize what has been done already.”
Essentially, the overall goal is, once treated, to get on board and start treating the patient more aggressively for osteoporosis.

Saint Luke’s Hospital Campus Medical Plaza Building 1, Ste 610, 4321 Washington St., KCMO
and at 3651 College Blvd, Leawood, KS 66211
913.319.7600 | DD-Clinic.com






