A Clear View of Common Retinal Diseases Affecting Vision

It is important to be aware of the warning signs of eye disease that could lead to vision loss if left untreated.
If we all are lucky enough to live a long life, we will most likely encounter some issues with our eyes. Around the age of 40, vision begins to change. Perhaps reading glasses are in order or you might have trouble adjusting to glare or distinguishing certain colors. All of this is a normal part of aging, but they do not have to keep you from enjoying an active lifestyle or hinder your independence. It is possible to live well into the afternoon of life and never experience significant vision loss, but as we age, we are at an increased risk of developing age-related diseases of the eye and other eye conditions. By age 65, one in three Americans will have some form of vision-impairing eye disease, and this also includes diseases directly related to the retina.
Diseases of the retina, which can occur at any point in our lives, are most common as we age, and a healthy retina is vital for good vision. The retina is the thin membranous lining at the back of the eye. This light-sensitive nerve tissue controls how images are viewed. The images are focused at the retina and converted to electrical impulses which are then carried to the brain by the optic nerve.
While there are several diseases and issues that affect the retina, the most common include age-related macular degeneration, diabetic retinopathy, and retinal detachment. Retinal diseases vary, but the majority of them cause visual issues that can affect any part of the retina. Treatment is available for many retinal diseases and, depending upon one’s condition, treatment goals may be to either stop or slow the disease and preserve, improve or restore vision. Left untreated, some retinal diseases can cause severe vision loss or even blindness.
Among the most common symptoms of retinal disease include seeing floating specks or cobwebs, flashes, blurred or distorted vision, defects in side vision or lost vision. As we age, it is important to pay close attention to any changes in our vision and seek medical care immediately if you experience any of these symptoms.
Dr. Blake Cooper, M.D. and vitreoretinal surgeon with Retina Associates in Shawnee, Kansas, treats patients for eye diseases primarily affecting the retina. Dr. Cooper indicated one of the most prevalent age-related diseases of the eye is macular degeneration, which can present in both dry and wet forms. Roughly 90% of those with age-related macular degeneration (AMD) have dry AMD, a condition that affects the layers of the macula, in which they become thinner over time, function less as they do, essentially atrophying. In the early stages, tiny drusen, which are piles of waste product of the cells of the eye, appear under the retina. Drusen may lead to deterioration of the retina, but dry AMD usually does not progress to severe visual loss.
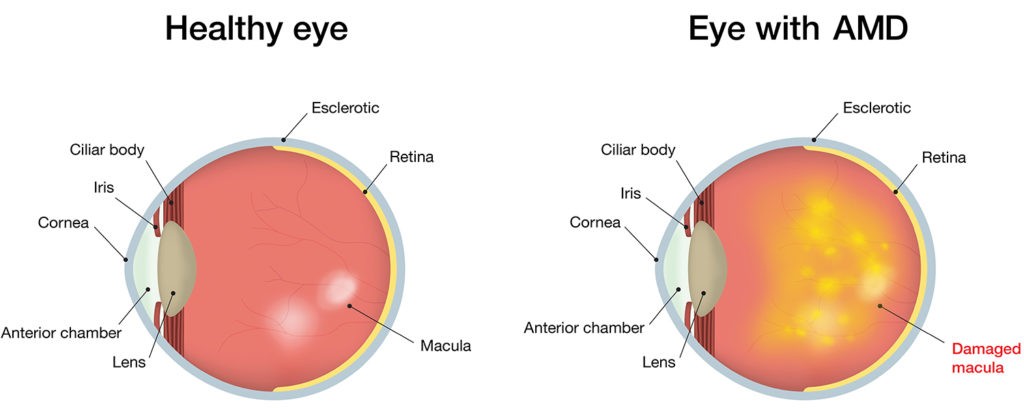
On the other hand, wet AMD, seen in about 10% of all cases of AMD, is a condition involving the growth of new blood vessels in the choroidal layer under the retina. Because the new vessels are weak, they can leak fluid and blood. As the leakage seeps into the layers of the retina, scar tissue can form and the retinal cells will cease to function. Of the two, dry AMD is more common and less severe. Early detection and treatment of dry or wet AMD can help reduce vision loss and in some cases, perhaps recover vision.
“By age 85, 40% of the population has AMD,” stated Cooper.
In short, macular degeneration can dramatically affect the central vision. While people rarely go blind because of this disease, it can be challenging to read, drive or perform normal functions of everyday living. Located in the center of the retina, the macula is the light-sensitive layer of tissues at the back of the eye. As it deteriorates, disease results. One of the most common methods of treatment for macular degeneration is laser surgery.
To reduce your risk of AMD, Cooper emphasized the importance of taking measures to keep your blood pressure under control and to quit smoking if you have the habit. These two steps alone will help to slow down the progression of the disease. Further, after age 65, it is vitally important to have an annual dilated eye exam. By age 85, roughly 40% of the population will develop ARM and it tends to be more prevalent in females than in males, according to Dr. Cooper.
Changes in diet can also be effective and this includes the incorporation of vitamins. Cooper recommends AREDS 2 (age-related eye disease study) vitamins to patients who have moderate to advanced stages of macular degeneration.
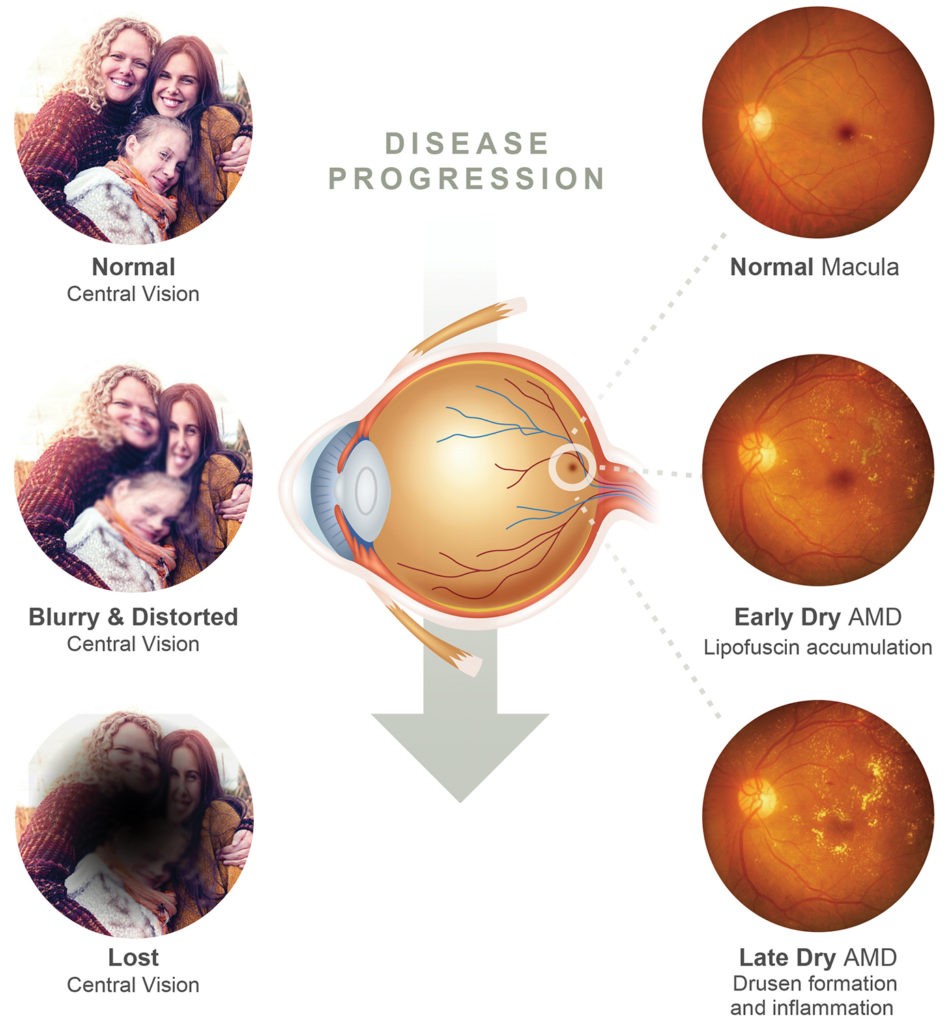
“Macular degeneration is a progressive condition and it can get worse over time,” Cooper indicated. “You can lose color contrast and clarity, but not all of your vision. You may not be able to read well or pass a driver’s test, but there are various visual aids you can use to assist your vision.”
Another common retinal disease is diabetic retinopathy, something about which every diabetic should take heed.
“Within the general population, if you are not experiencing any visual problems, we recommend getting a thorough eye exam every three to five years,” emphasized Cooper. “For diabetics, we recommend an annual comprehensive eye exam and also taking steps to control the risk factors, such as elevated blood sugar, blood pressure and cholesterol levels.”
Diabetic retinopathy, a potentially blinding disorder resulting from diabetes, causes abnormal changes in the blood vessels of the retina. As these blood vessels weaken, they can leak fluid into the layers of the retina, close off or even hemorrhage. As these vessels break down, new ones may form that can contract and can detach the retina. Consistent high blood pressure and high blood sugar are associated with diabetic retinopathy. While there is no cure for this disease, laser treatment, intravitreal injections, or surgery is usually effective at preventing vision loss, especially if performed before severe damage of the retina occurs.
With diabetic retinopathy, Dr. Cooper explains a patient may remain asymptomatic until the later stages. He or she may be able to see well but is unaware of changes going on within the eye that can affect his or her vision over time.
“Microvascular damage could be happening without their realization and it is important to determine if that is occurring so treatment can begin to stall the progression of the disease,” noted Cooper.

Dr. Cooper strongly supports patient education and awareness, and this is important with all diseases of the eye, especially one as time-sensitive as a retinal detachment, an emergency situation in which a thin layer or tissue – the retina – pulls away from the layer of blood vessels that support it with oxygen and nutrients.
A serious eye disease, the risk factors for a retinal detachment include severe nearsightedness; a previous eye injury or cataract surgery; or a family history of retinal detachment. The primary symptoms include seeing flashes of light; noticing lots of new floaters, and the darkening of your peripheral vision, as if a curtain is being drawn closed. The presence of any or all of these symptoms necessitates an immediate call to an eye care specialist. While floaters and flashes are quite common as we age, typically in our 60s and 70s, the presence of new flashes and floaters – especially in large quantities – may indicate a retinal tear and/or detachment, and this requires a fully dilated eye exam to determine the extent of the problem. Once identified, a retinal detachment should be repaired in a timely manner. If holes or tears in the retina are found before the retina detaches, the eye doctor can close the holes using a laser, and this can usually be performed within the doctor’s office setting. The sooner a retinal detachment is addressed, the better chance the patient has of vision being restored.
Another common eye disease is glaucoma, which affects the optic nerve, unfortunately offers no obvious symptoms initially to the patient. (Hence, another reason to get an annual eye exam!). As the disease advances, however, the person with glaucoma may notice that side vision is gradually failing. There are a variety of medications used to treat glaucoma, and these include eye drops or pills. However, medications alone do not control the eye pressure in some patients. As a result, surgical intervention may be necessary. A common type of surgery – trabeculoplasty – uses a laser to improve the flow of fluids out of the eye. This can usually be done in the doctor’s office. Trabeculectomy, a conventional surgery, involves the doctor creating a new drainage path in the eye, under the eyelid. Risk factors for glaucoma include age, family history of the disease, the use of steroid medications and near-sightedness.
Yes, as we age, things do change, and our eyes are no exception. However, healthy habits to keep your eyes and vision at optimum levels include getting regular eye exams, practicing eye health prevention; maintaining a healthy lifestyle; quitting smoking (and certainly don’t start!); wearing sunglasses; resting your eyes and wearing eye protection when needed. Eye diseases can only be fully diagnosed through a comprehensive exam by an ophthalmologist, and that exam should include at least a visual acuity test; pupil dilation; and tonometry, a standard test used to determine the fluid pressure inside the eye. Of all our primary senses, our sense of sight is certainly one to cherish.
Sources: asrs.org, mayclinic.org, agingcare.com, aao.org, webmed.com.







