Brain Injury Awareness Month

Raising awareness and helping to eliminate the stigma around brain injuries.
 One in every 60 people is living with a permanent brain injury-related disability. This may be you or someone you know. Unfortunately, brain injuries are often misdiagnosed, misunderstood, and represent an underfunded neurological disease.
One in every 60 people is living with a permanent brain injury-related disability. This may be you or someone you know. Unfortunately, brain injuries are often misdiagnosed, misunderstood, and represent an underfunded neurological disease.
According to the Brain Injury Association of America (BIAA), brain injury is a leading cause of death and disability in the United States. At least 2.8 million Americans experience a traumatic brain injury (TBI) every year. Brain injuries can be sustained from a fall, being struck by or against something, from car accidents, from assaults, and from unknown causes. A brain injury can also be the result of a stroke, infectious diseases, and brain tumors. Mild TBIs are typically the result of concussions.
With March as Brain Injury Awareness Month, it is a good time to further understand how brain injuries occur, what we can do to reduce our chances of suffering from one, and how those who unfortunately sustain a brain injury can be helped.
“So many things can lead to a traumatic brain injury,” noted Dr. Sushma Lueder, Director of the Brain Injury Rehabilitation Program at MidAmerica Rehabilitation Hospital (MARH). “A traumatic brain injury is any type of trauma that happens to your brain that will disrupt its natural function. This can be the result of a car accident, a bicycle or motorcycle accident while not wearing a helmet, falling off a ladder while working around the house, or slipping and falling on the ice, among many other things.”
Concussions occur more often than one might think. Sudden jolts or bumps can cause the brain to bounce back and forth in the skull.
This can cause injuries of various degrees. Symptoms of  concussions may include dizziness, nausea, ringing in the ears, and headaches. Other symptoms may include difficulties in sleeping or depression and anxiety. Most individuals who sustain a concussion typically recover in a few days or weeks. For others, it might take a bit longer.
concussions may include dizziness, nausea, ringing in the ears, and headaches. Other symptoms may include difficulties in sleeping or depression and anxiety. Most individuals who sustain a concussion typically recover in a few days or weeks. For others, it might take a bit longer.
Although most people associate concussions with youth sports and professional athletes, older adults are highly susceptible to a concussion just from falling. In fact, Harvard Medical School reported that a common cause of hospitalization among those age 65 and older is the result of a fall. To minimize the risk of falling to seniors, proactive steps can be taken that include removing hazardous throw rugs; adding additional light to spaces to help avoid any tripping; installing handrails and grab bars; staying active, and wearing sensible shoes.
For active individuals of all ages, helmets help to prevent TBIs. It is highly suggested you wear a helmet when you are on a motorcycle, bicycle, or horse or when you participate in sports such as football, hockey, lacrosse, skiing, roller skating, skateboarding, snowmobiling, and snowboarding.
It is strange to think, too, that an autopsy on the late actor/comedian Bob Saget, who unexpectedly passed away in January, revealed he died from head trauma. An article printed in People Magazine reported that authorities concluded he sustained a head injury after accidentally hitting his head on the back of something, did not think much of it, went to sleep, and never awakened. That is how simply a brain injury can occur, and, sadly, how deadly it can be.
Dr. Lueder emphasized the importance of consulting with a physician after sustaining a head trauma of any kind, especially if the patient or family members sense something is off with the patient and things aren’t functioning as normally as they should. When you see a doctor for a suspected brain injury, you are then on his or her radar. Care has been established and the doctor now has a history of your incident.
Dr. Lueder indicated some symptoms that can give rise to suspicions of traumatic brain injury include headaches, dizziness, nausea, poor coordination, change in vision, memory issues, difficulties in problem-solving, having slow mental processing, drowsiness, inability to concentrate, or weakness or sensory deficits on one side of the body.
Another type of brain injury that one can sustain is considered non-traumatic. The term for this is encephalopathy. I’m bringing this to attention because we care for quite a few encephalopathic patients. Encephalopathy typically occurs in critically ill patients with systemic illness, examples include but are not limited to UTIs, pneumonia, liver or kidney failure or COVID-19 infection. It consists of delirium and an acute confusional state. It is defined as a condition of global cerebral dysfunction in the absence of primary structural brain disease. There are multiple etiologies that can cause encephalopathy, such as cerebral edema, medication induced delirium, electrolyte derangement or lack of oxygen to the brain. Those that are at highest risk of acquiring an encephalopathy are the elderly and patients with an underlying dementia. A few findings in these patients are decreased attention, cognitive deficits, disturbance in sleep-wake cycle and also decreased alertness.
 In her practice at MARH, Dr. Lueder places a strong focus on activities of daily living and mobility with her TBI patients, who may experience difficulties with gait, balance, bathing, dressing, and grooming. Our goal is to improve our patients daily function and quality of life.
In her practice at MARH, Dr. Lueder places a strong focus on activities of daily living and mobility with her TBI patients, who may experience difficulties with gait, balance, bathing, dressing, and grooming. Our goal is to improve our patients daily function and quality of life.
“We deal with this decline in everyday function with patients who have TBIs,” she expressed.
Dr. Lueder further explained that typically patients who sustain mild to moderate TBIs tend to recover well. However, those with a more serious brain injury tend to have a more challenging road to recovery.
“The more severe the brain injury, the more significant the deficits. However, the younger the patient is, the better the recovery,” she stated.
At MARH, patients have access to acute in-house services through a multi-disciplinary approach. This includes physical therapy, occupational therapy, speech therapy, case management, and assignment to a rehabilitation doctor.
“All of these disciplines provide a great start to recovery, and while not everyone will recover fully, they can each gain a different level of independence,” said Dr. Lueder.
Among the highly innovative and advanced technologies implemented at MARH to assist patients with TBIs include the Bioness system, which helps weak extremities that have lost functional usage, increased motion and improving walking. The Bioness Integrated Therapy System (BITS) challenges and assesses physical, visual, auditory, and cognitive abilities. The activities used therein evaluate reaction time, auditory and visual processing, memory, physical and cognitive endure and visuospatial perception. Because patients can track their progress, they tend to become quite motivated to improve. Also, electrical stimulation of the facial muscles and swallow muscles via the Vital Stim technology aids in retraining muscle groups to improve the function of swallowing.
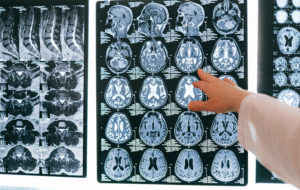
Through the use of comprehensive brain testing tools and technologies in conjunction with rehabilitation therapy and other treatment protocols, patients, together with their healthcare providers, can work towards the best possible outcomes.
Sources: biausa.org,macconcussion.com






