National Breast Cancer Awareness Month

Story by Jeanie Edgmon
 We want to dedicate this article to the late Dr. Kelley Lynn Young April 18, 1975 – June 15, 2021 who fought a courageous battle against breast cancer. Many of our readers are familiar with her dedicated work as founder of MISH Hospital and Clinics Cancer and Blood Center. Dr. Young was a cover feature of Healthy Kansas City in March of 2017 and created a wide impact within the community implementing the latest knowledge and technologies to fight cancers while keeping relationships of the highest priority. While we have lost a friend, we will continue to feel her legacy and be blessed by her efforts within the Kansas City area for generations to come. May we all fight on for Dr. Young and all those affected by breast cancer.
We want to dedicate this article to the late Dr. Kelley Lynn Young April 18, 1975 – June 15, 2021 who fought a courageous battle against breast cancer. Many of our readers are familiar with her dedicated work as founder of MISH Hospital and Clinics Cancer and Blood Center. Dr. Young was a cover feature of Healthy Kansas City in March of 2017 and created a wide impact within the community implementing the latest knowledge and technologies to fight cancers while keeping relationships of the highest priority. While we have lost a friend, we will continue to feel her legacy and be blessed by her efforts within the Kansas City area for generations to come. May we all fight on for Dr. Young and all those affected by breast cancer.
Each year since 1985, October has been set aside as National Breast Cancer Awareness Month. It has become one of the most recognized and successful annual health campaigns in the United States. This is fitting and necessary as breast cancer is the most common cancer in American women, except for skin cancers. The average risk of a woman in the United States developing breast cancer sometime in her life is about 13%, or 1 in 8 women being diagnosed in her lifetime. Each year, an estimated 281,550 new cases of invasive breast cancer will be diagnosed in women. About 49,290 new cases of ductal carcinoma in situ (DCIS) will be diagnosed. Tragically, about 43,600 women will die from breast cancer.
While those statistics are startling and real, it is equally important to know that we are making significant progress.
According to the American Cancer Society, breast cancer death rates have declined an astounding 40% from 1989 to 2016 among women. This progress was primarily attributed to improvements in early detection.
Unprecedented Challenges Brought Unprecedented Advances
And we are likely to soon see many more advancements stemming from an unlikely event – the worldwide COVID pandemic. The pandemic caused an unprecedented level of scientific collaboration in the development of the Covid-19 vaccines, as well as on many other fronts, including cancers. The American Association for Cancer Research reports that in this time, twenty-one novel oncology drugs were approved by the U.S. Food and Drug Administration (FDA) in 2020, including for difficult-to-treat cancers such as triple-negative breast cancer. It is hopeful that this new more collaborative environment will continue and advance the prevention, detection, and treatment of breast cancer. On April 22, 2020, the Food and Drug Administration granted accelerated approval to sacituzumab govitecan-hziy (TRODELVY, Immunomedics, Inc.) for adult patients with metastatic triple-negative breast cancer who received at least two prior therapies for metastatic disease. The FDA also approved a number of targeted therapies to treat HER-positive breast cancer including a drug called Margenza.
Additionally, the first liquid biopsy next-generation sequencing tests were recently approved. Liquid biopsies are being used more frequently in managing breast cancer as well as other types of the disease, such as lung cancer. However, as do all treatments, liquid biopsies do have limits. One study has found that most of the mutations found through the test came from white blood cells and not cancer cells. We need continued research to know more definitively the best way to use liquid biopsy to help treat breast cancer.
During the height of the pandemic, many clinical trials ceased without the opportunity for in-person visits. This caused another unexpected change likely to impact the future of breast cancer research. The unavailability of face-to-face meetings forced clinical researchers to determine which procedures are absolutely necessary to do in person and which can be completed remotely. Long-term, these remote procedural changes may widen the availability of people available for trials.

Advances in Imaging
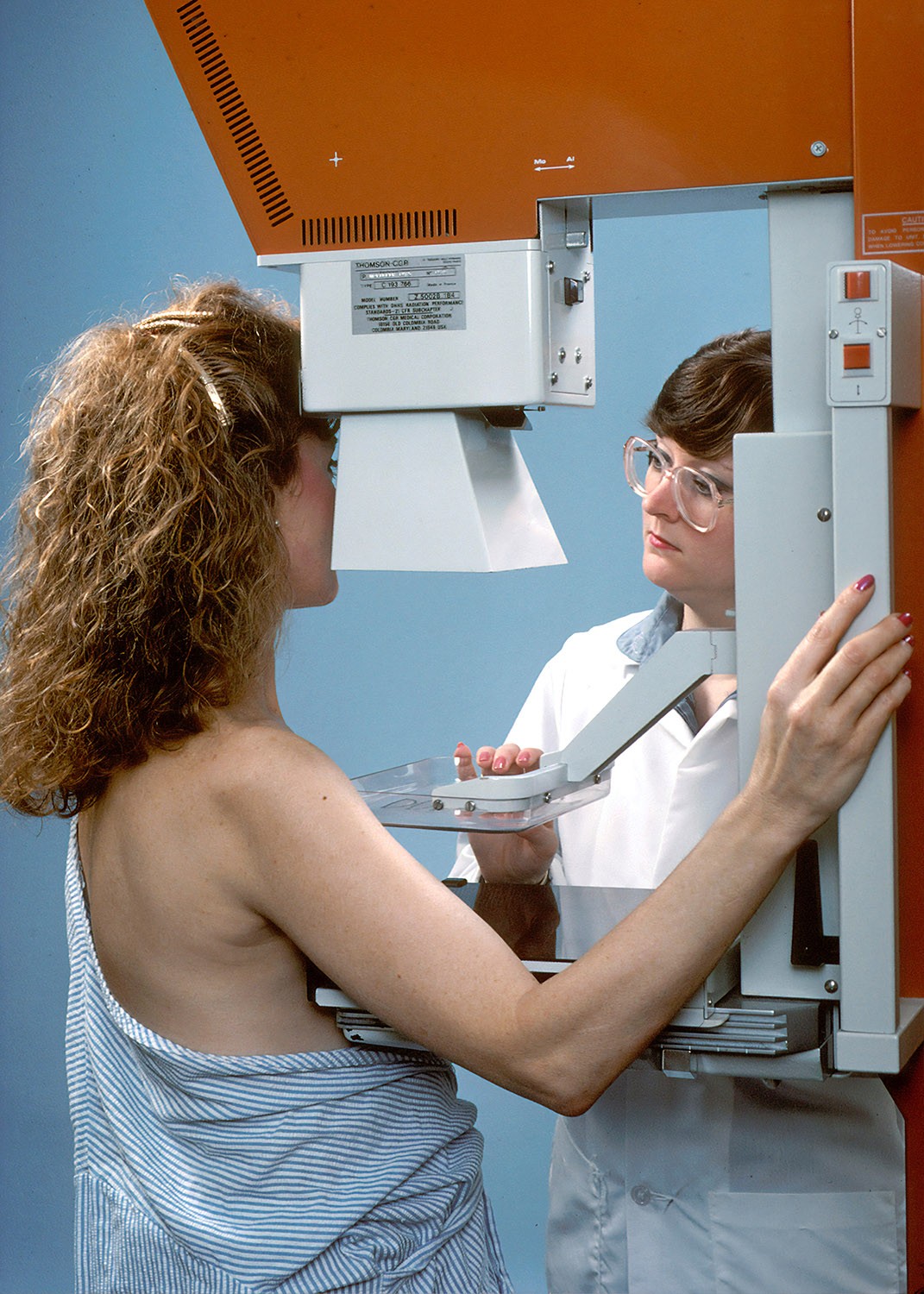
Although currently conventional mammography remains the primary screening tool for breast cancer and has been shown to reduce breast cancer mortality, it too, has limitations. The most common limitation is of low sensitivity, specificity in women with dense breast tissues.
Fortunately, increased options in better imaging may change the way we diagnose and treat breast cancer. Recently, research has been conducted aimed at evaluating a new digital breast tomosynthesis (DBT)/DOT fusion imaging technique and obtaining preliminary data for breast cancer detection. Researchers hypothesized that DBT/DOT fusion imaging would be useful for breast cancer diagnosis particularly in dense tissue, with the technique combining both the morphological features provided by DBT and the functional information provided by DOT. Early research shows significantly higher diagnostic performance in this area.
Better optical imaging could also reduce the need for additional surgeries in cancer patients. Many patients with early-stage breast cancer undergo breast-conserving surgery, which involves local removal of cancer with a surrounding margin of healthy tissue. The goal is to remove the entire tumor while preserving the healthy tissue. Excision, however, is primarily based on visual inspection and heavily relies on the surgeon’s expertise. Roughly 20% of patients require a second surgery due to incomplete initial removal of cancerous tissue, according to Physics World. A team at Thayer School of Engineering at Dartmouth and Dartmouth-Hitchcock Medical Center is investigating whether Optical Scatter Imaging could help.
Using AI in Reading Mammograms
A recent JAMA Oncology study found that an artificial intelligence (AI) algorithm was as accurate as, or better than, an average radiologist at identifying breast cancer on screening mammograms. The AI had a sensitivity of 81.9% compared with a sensitivity of 77.4% for a first-reader radiologist. When a first-reader radiologist was paired with the AI, their ability to detect breast cancer was even greater, with 88.6% sensitivity at 93.0% specificity. Though initial studies show that expert physicians paired with AI improved diagnostic performance, the clinical implications are uncertain.

Personalized Treatments
One of the most significant recent advances in breast cancer treatment is personalized treatments. Increased research has fundamentally shifted the way cancer is treated with a new understanding that women with the same type of cancer may respond very differently to the same treatment based on a number of factors.
The identification of risk factors through things such as genetic testing that look for hereditary cancers can help avoid the development of cancer, encourage early detection and guide treatment. Better imaging is also playing a role in monitoring the effectiveness of treatments so that they may be guided more precisely.
This Year Awareness is Even More Important
Breast Cancer Awareness Month is a good time to take stock of all the advances of the previous year and mark the progress we’ve made against this disease. This year, stopping to shed additional light on breast cancer may be even more important. Studies show that one in three women have delayed mammograms due to the COVID-19 epidemic and half are reluctant to visit their doctor. Travel restrictions, practice reduction, limitations to non-urgent care, and treatment postponement and changes also had a significant impact on breast cancer detection and treatment over the last year.
The last year has been a powerful reminder of the importance of collaboration, dedication, and advocacy. More than ever, it is important to encourage the women in our lives to get screened for breast cancer.
Visit the National Breast Cancer Foundation nationalbreastcancer.org/breast-cancer-awareness-month





