Rockhill Orthopaedic Specialists Has Many Options for Their Patients
Advanced Techniques and Emerging Technologies in Orthopaedics
Portrait photos by Matt Kocourek
Pictured above left to right: Alan Zonno, M.D., Megan Mayer, M.D. and Andrew Palmisano, M.D.
Rockhill Orthopaedics prides itself in always being at the forefront of introducing new technologies to improve patient care. Their innate ability to use advanced techniques and emerging technologies enables them the best means to serve their patients.
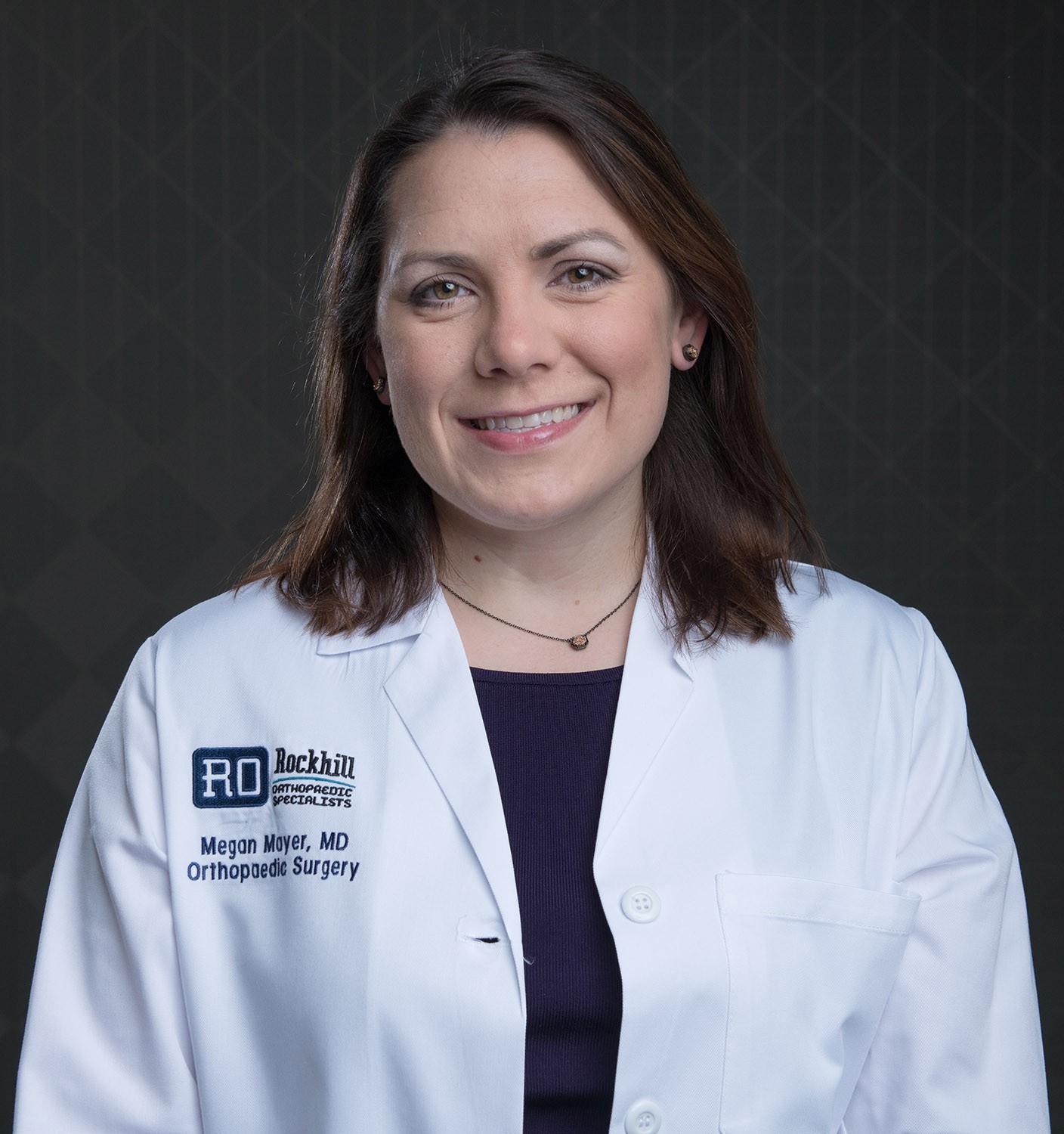
Hip Pain – What are my Treatment Options with Megan Mayer, M.D.
Dr. Mayer is a fellowship trained board eligible orthopedic surgeon specializing in hip, knee and shoulder arthroscopic procedures as well as Sports Medicine, employing the most current treatment techniques to alleviate pain and restore function and an active lifestyle for her patients.
Over the past decade, treatment options have changed dramatically for hip pain. Attaining a proper and timely diagnosis of your hip pain is vital, as treatment options may vary, depending on the root cause of your discomfort. Many patients visit multiple physicians before they can narrow down an accurate diagnosis. This can be reduced by seeking a hip specialist like Dr. Megan Mayer with Rockhill Orthopaedic Specialists. She is a dedicated Hip Arthroscopy and Sports Medicine Orthopaedic Surgeon.
Hip Conditions
- Hip Impingement or Femoroacetabular Impingement (FAI) – Mismatch in the shape between the ball and socket of your hip joint.
- Labral Tear – A tear in the ring of the cartilage around the socket, commonly seen in athletes. Often accompanies impingement.
- Arthritis – Degenerative or inflammatory process that leads to breakdown of the cartilage that cushions your hip joint.
- Bursitis – Bursae are fluid sacs that combat friction around the joint. Bursitis is inflammation of the bursae.
- Tendonitis – Inflammation of the tendons.
- Stress Fracture – Stress reaction in the bone due to overuse. Needs timely evaluation to prevent additional injury.
According to Dr. Mayer, conservative, non-surgical treatment is always part of the discussion with her patients regarding treatment options for hip pain.
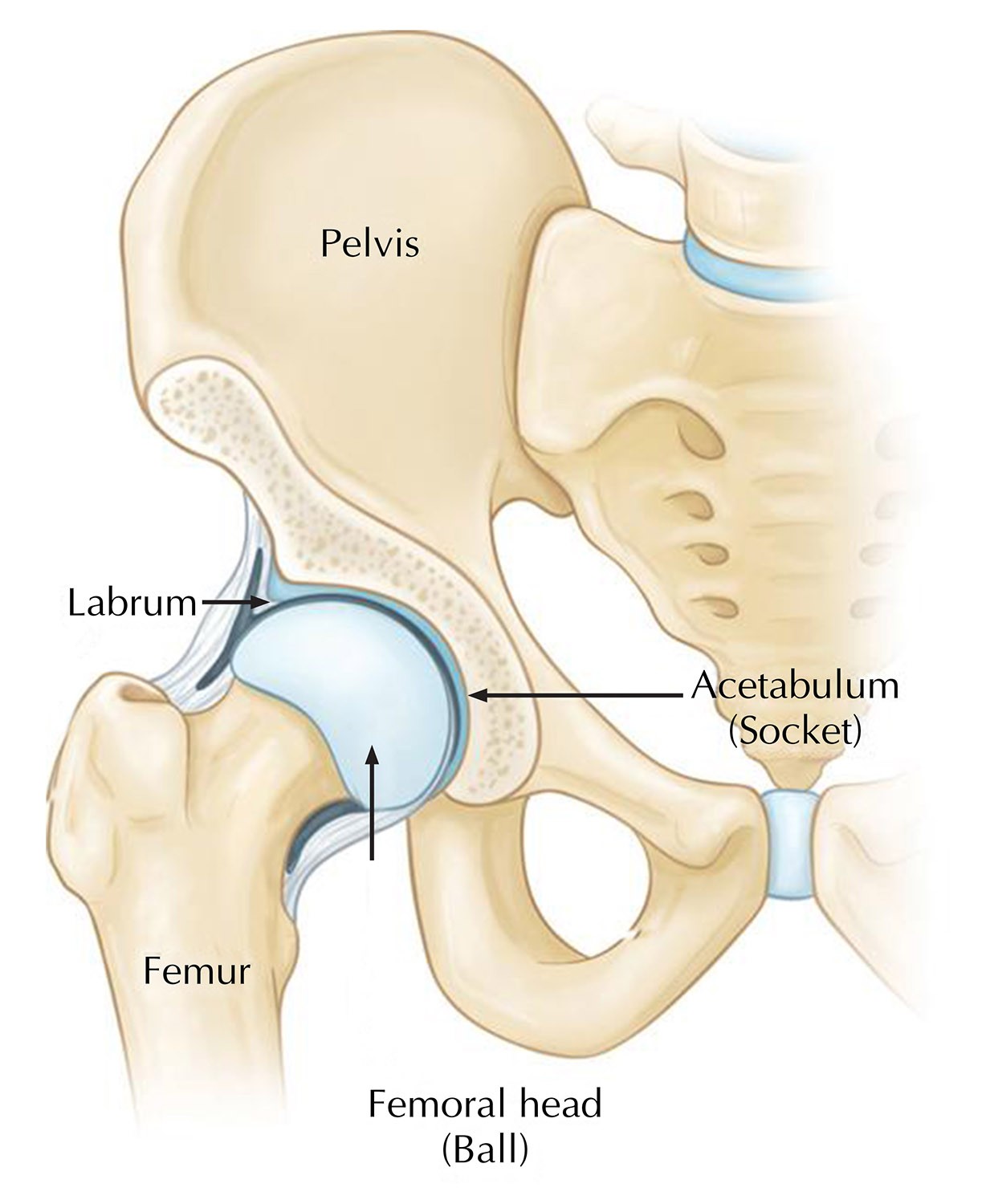
Photo courtesy of OrthoInfoaaos.org
Types of nonoperative treatment could include:
- NSAIDS-Non-Steroidal Anti-inflammatory Medications
- Activity Modification
- Physical Therapy-strengthening, stretching & flexibility
- Manual Therapy Interventions-soft tissue mobilization
- Gait Training & Balance Coordination
- Use of Orthotics
- Injections
Conservative treatment can lead to decreased pain, improvement in functional movement, and increased lower extremity muscular balance. Patients who are non-responsive to treatment, may be offered a cortisone/steroid injection into the hip joint to see if the pain can be relieved and confirm the hip joint as the source of the pain. However, if the patient has no decreased pain, the problem may be originating from a tendon or a muscle around the hip joint or it could be referred pain coming from the back. When conservative management fails, surgical treatment options are available.
Surgical Treatment Options
Surgical options for patients with structural hip pain originating from the hip and surrounding hip region have evolved over the years. Procedures range from Hip Arthroscopy to open surgical procedures, including joint replacement, depending on the pathology. Surgical treatment for impingement addresses structural abnormalities by removing the source of friction between the bones of the hip joint, preserving the joint and slowing arthritis. When hip pain is due to more advanced arthritis, total joint replacement is an option. Dr. Mayer specializes in hip arthroscopy with the goal to preserve the native hip joint and maintain patients’ activity levels.
Arthroscopic surgical hip procedures have significantly improved over the years and are available as outpatient, in which, the patient goes home the same day and the complications are greatly reduced compared to open procedures for hip impingement.
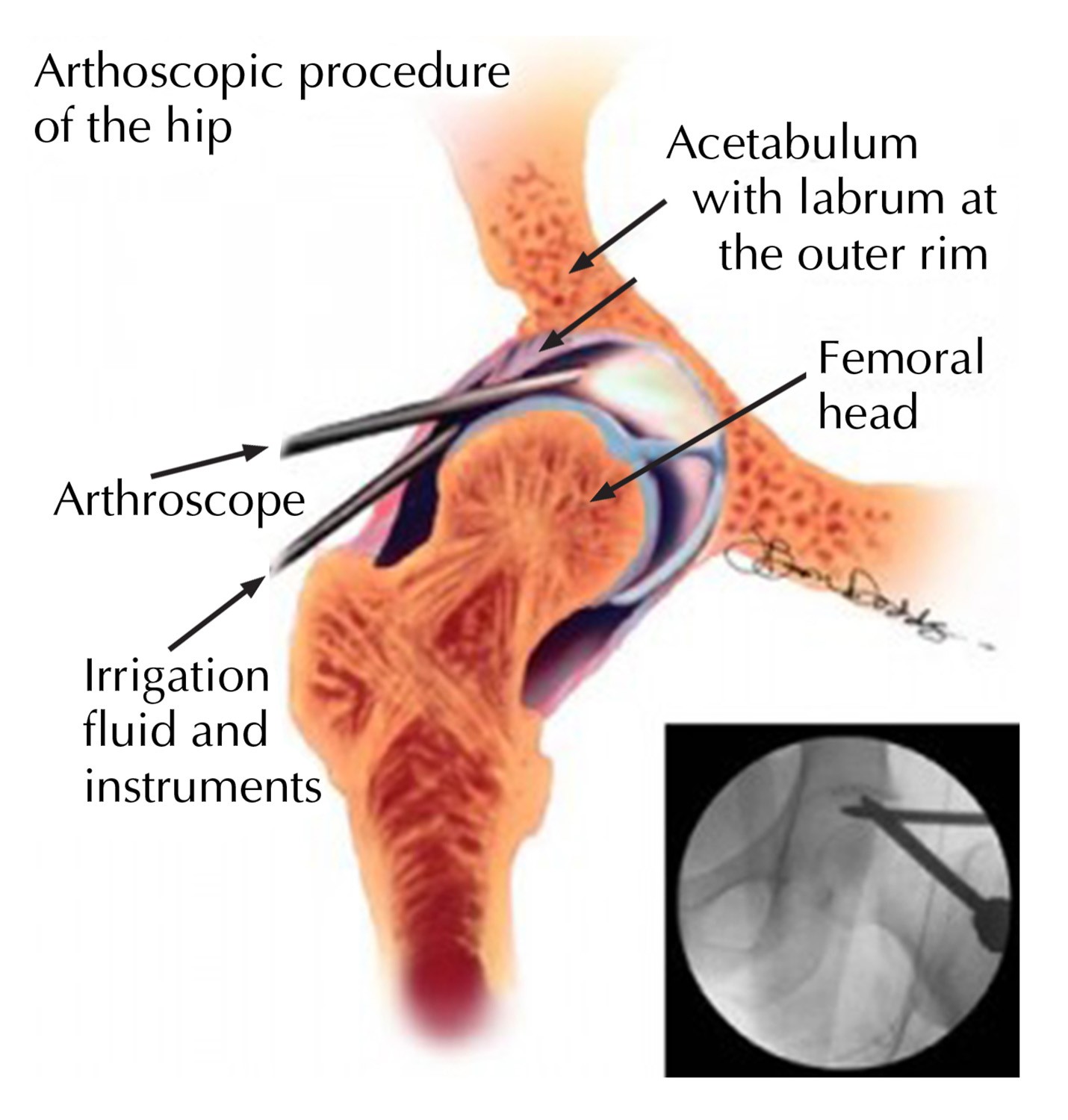
Photo courtesy of OrthoInfoaaos.org
Hip Arthroscopy
Hip arthroscopy, involves inserting a small camera, called an arthroscope, into your hip joint through tiny incisions. The surgeon can then visualize the hip joint on a video monitor and guide small specialized surgical instruments to correct the structural deformity. Dr. Mayer can smooth and/or repair torn cartilage, trim off bone causing hip impingement, and remove synovial connective tissue that has become inflamed. Overall, with an appropriate rehabilitation process, patients can often return to full activities after arthroscopy. In fact, many hip arthroscopy patients can return to their normal physical activity and sports at the same level of competition they were before surgery. However, if hip pain is left untreated, arthritis may ensue and progress to the point where a total hip replacement becomes the best treatment option.
Dr. Mayer is compassionate with her patients and takes time to thoroughly evaluate their complaints and discuss treatment options. Her goal is to preserve the hip joint and get patients back to the activities they enjoy.
Contact our office for a consultation with Megan Mayer, M.D. about your hip pain, call (816)-246-4302

Ready for a Total Joint Replacement with Andrew Palmisano, M.D.
Dr. Palmisano is at the forefront of advanced techniques for the surgical treatment of bone and joint problems, including: arthritic and inflammatory conditions, degenerative problems, failed joint surgeries/revisions, infected joints and AVN-avascular Necrosis, (blood flow problem) of knee and hip.
Osteoarthritis is a degenerative process, that causes damage to the affected joint when the cushion between bones (cartilage) breaks down, making joints painful and hard to move.
Age, previous joint injury, obesity, weak muscles, genetics and being female are all contributing factors for developing osteoarthritis.
Treatment options start with conservative non-invasive simple options such as:
- NSAID-Non-Steroidal Anti-inflammatory Drugs
- Physical Therapy
- Limited weight bearing activities
- Weight Loss
- Corticosteroid Injections
- Viscosupplement Injections (Gel)
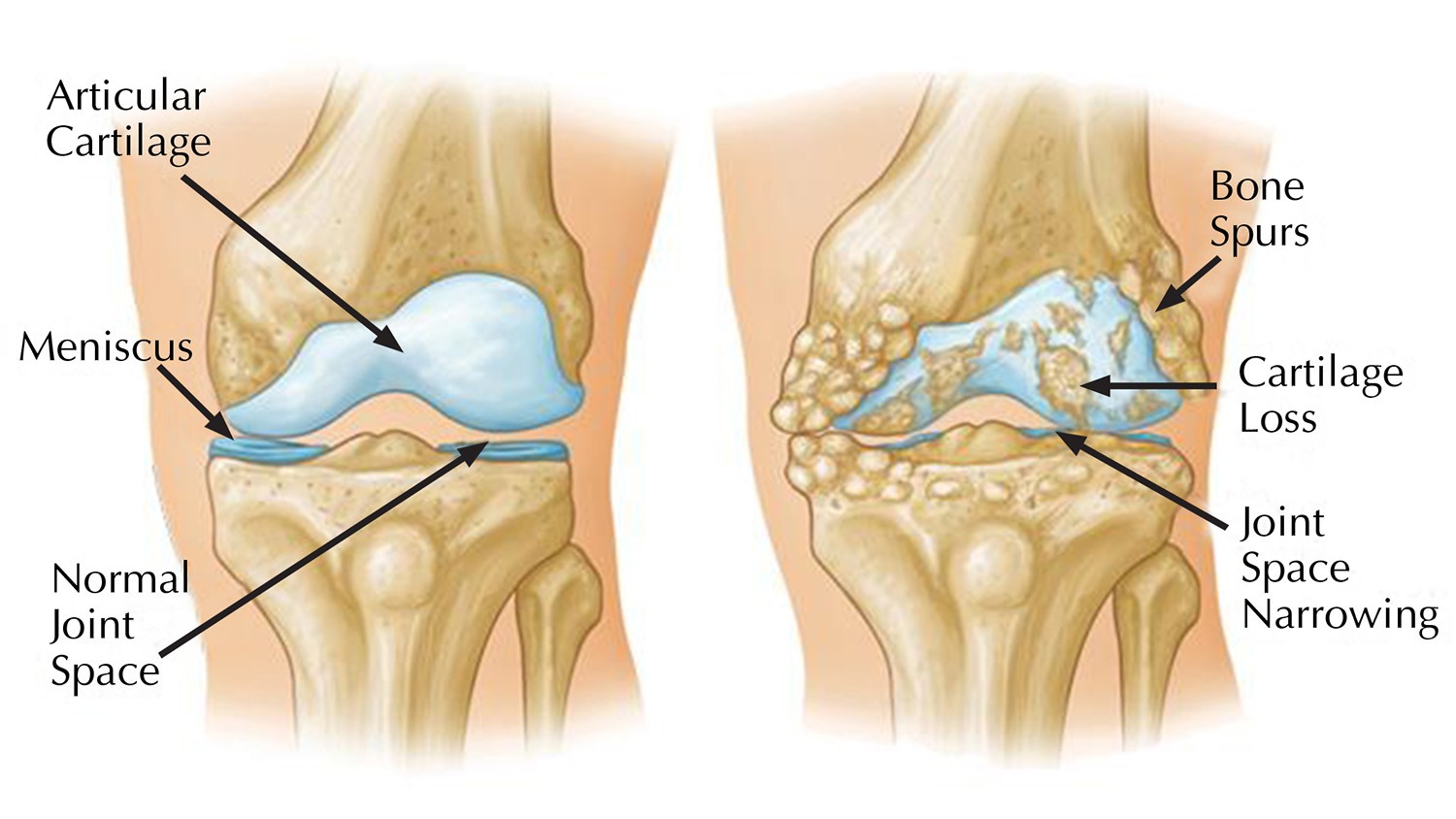
Photo courtesy of OrthoInfoaaos.org
When Is It Time?
Each person tolerates pain differently. Most people can tolerate joint pain for months to years. The pain slowly worsens as the arthritis worsens. It may be time to see a joint specialist when:
- Your pain limits daily activities as simple as walking or stairs
- Your joints are chronically inflamed or swollen
- You do not get relief from conservative options
- You have a deformity of your knees or hips (decreased motion or bow-legged stance for example)
Joint Replacement/Arthroplasty: Surgical removal of the damaged bone and cartilage and replace the joint with an artificial joint usually made of metal, plastic and ceramic.
Modern medicine has many great successes and hip and knee replacements are two of them. There several options available for each joint depending on situation (XR, pain, deformity) of the patient. This conversation can be started with your surgeon at any time, well in advance of when you are ready for surgery. It never hurts to become more informed of options for your situation.
In-Patient vs Out-Patient Surgery?
Rockhill Orthopaedic Specialists Total Joint Program is a comprehensive clinical management program, which is geared towards clinical outcomes that meet the highest quality metrics. Our program includes, pre-operative patient education, physical therapy prior to your surgery and after, open communication through the process and scheduled follow up visits. “As the Medical Director I have spent years developing a program to provide the best outcomes possible for our patients.”
“As modern medicine advances, the times of 5 day hospital stays after joint replacement are a thing of the past. We use tested rehabilitation protocols that allow patients to get up and walk with limited pain the day of surgery. We can discuss options for timing and location of surgery depending on your personal situation,” noted Dr. Palmisano.
Outpatient: Certain patients may be better suited for outpatient surgery performed at a surgery center in which you avoid exposure to the hospital setting and are discharge the same or next day.
Inpatient/Inhospital: For those patients that need a little more help or have other complicating medical conditions surgery performed at the hospital may be a better option.
Throughout your surgical experience there are many team members that are all trained to help you have the best outcome possible. As the joint specialist I may lead the team however, this surgery is not possible without a large team including, nursing staff, anesthesia providers, schedulers, office staff, physical therapists and advanced practitioners, (Physician Assistants/Nurse Practitioners) all working together.
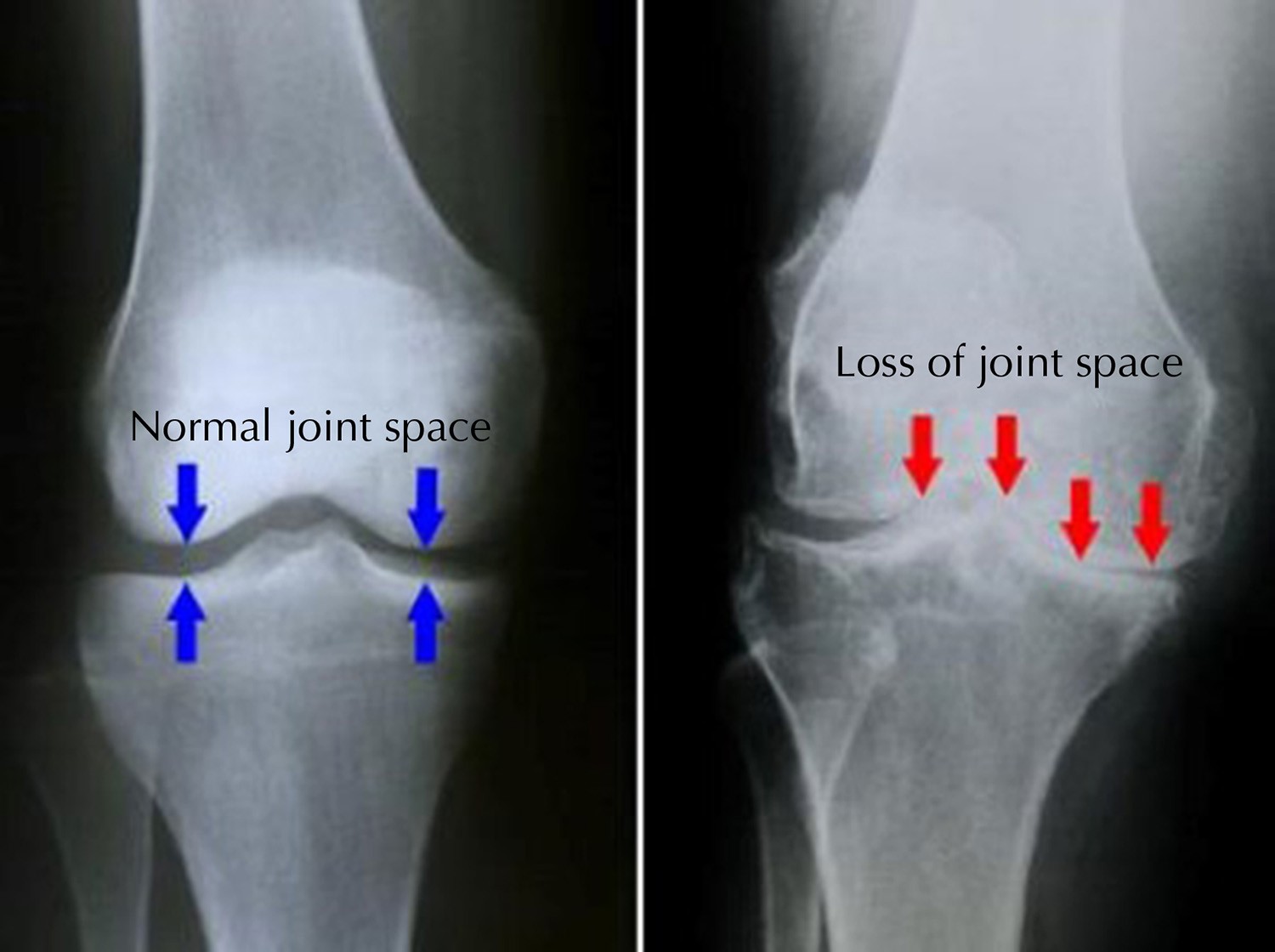
Photo courtesy of OrthoInfoaaos.org
Revision Joint Replacement?
Hip and knee replacements are two of the most successful procedures in all of medicine. In the vast majority of cases, it allows people to live richer more active lives free of chronic pain and disability. Over time a joint replacement may fail or become painful for a variety of reasons. Hip and Knee replacements should be checked every 1 to 2 years to ensure their proper function. This also allows the doctor to find any potential issues prior to failure.
Failure of a Replacement
A replacement can “fail” for many reasons. The most common symptom is pain. This may be due to the parts wearing out, become lose to the bone, the ligaments or muscles failing, instability or even infection.
“Everyone wants to know how long their hip or knee replacement will last. It is important to realize that while there are averages, there can be large differences between patients. An average implant may last 20-30 years; however in some patients, implants could fail or become painful much quicker within years and need a revision surgery,” stated Dr. Palmisano.
If you have had a hip or knee replacement that has become painful you should have this checked by either your operating surgeon or by a specialist if they are not comfortable with revision surgery.
A revision surgery may be recommended for any of these reasons. In this procedure some or all of the parts may need to removed or changed to provide pain relief and better function. A revision surgery has the same goal as the first replacement – pain relief – however this is often a much more complex surgery. Revision surgery is not something every surgeon who performs joint replacements are comfortable with. A fellowship trained joint specialist is someone who has spent an extra year of training to be able to fix failed replacements.
Contact our office for a consultation with Andrew Palmisano, M.D. about your joint pain, call (816)-246-4302
The Complex Nature of the Foot and Ankle with Alan Zonno, M.D.
Dr. Zonno is an orthopedic surgeon who is board certified, with fellowships in both Orthopedic Trauma and Foot & Ankle Reconstruction. Dr. Zonno originally planned to become a neurosurgeon, but on the first day of his orthopedic rotation in medical school he assisted with a fracture reduction and was hooked on orthopedics from that point forward.
What does a patient do when they are told that no fracture is seen on X-rays, but still has pain and trouble walking?
The foot is a complex structure that contains in excess of 25 bones, 30 joints, and more than a hundred muscles, tendons, and ligaments that work together to help you walk, run and jump. Your ankle joint is comprised of the tibia and fibula (bones from the leg) and the talus, which is the bone on the bottom. If any of these bones or the surrounding structures are injured —the result is all too often pain with activity — after which it is essential to obtain an accurate diagnosis in order to formulate the best treatment plan.
When should I seek additional care for my foot and ankle pain?
- If you are not able to bear weight on the foot due to pain
- Have persistent pain with weight bearing for 2 – 3 days
- Have intermittent pain that is activity limiting for several weeks or more
- What else could be wrong with my ankle if no fractures are seen after taking X-rays?
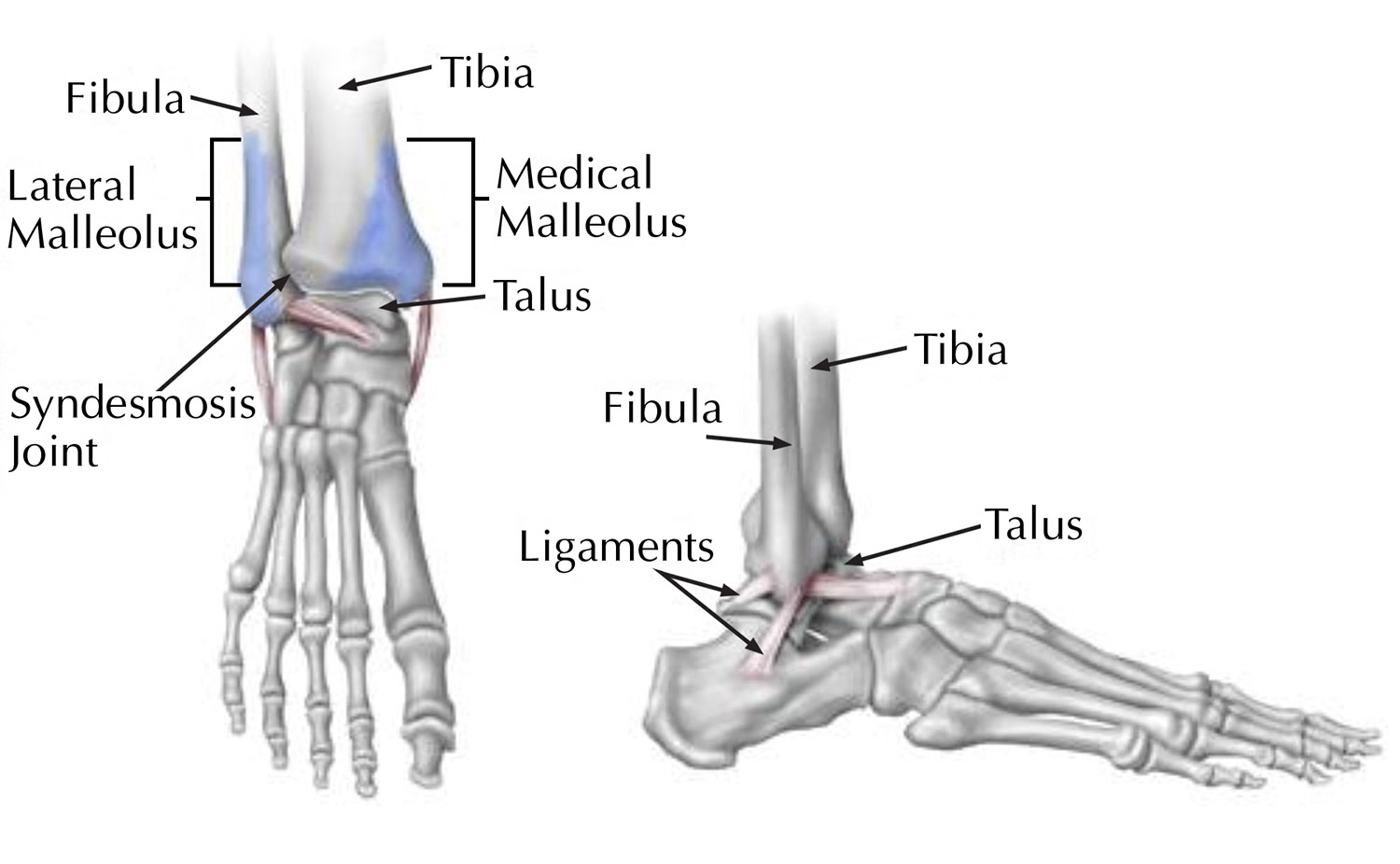
Photo courtesy of OrthoInfoaaos.org
Ankle Sprains
Ankle sprains occur when ligaments on the outside and/or inside of the ankle are stretched or torn and are responsible for the majority of ankle injuries without fractures. The vast majority of ankle sprains improve within three to four weeks using a typical “RICE” treatment protocol that stresses rest, ice, compression and elevation. Temporary rest includes activity modification to limit pain and may require immobilization in a splint, brace or walking boot. Ice can be used for 20 to 30 minutes at a time, three to four times a day, to reduce swelling. Compression (with an ace-wrap or pneumatic walking boot) and elevation (as much as possible for the first 24 to 48 hours) as well as use anti-inflammatory medications (such as ibuprofen or naproxen) can also help reduce pain and swelling. Ankle range of motion exercises are generally started within the first week to prevent stiffness. Strengthening and balance exercises are added as the pain and swelling subside — sometimes with the assistance of a physical therapist.
Is surgery required? Surgery is rarely required after most isolated ankle sprains. However, if instability persists despite appropriate physical therapy or if ankle sprains become more frequent, then surgical intervention may be required to tighten the ankle ligaments. Abnormal alignment of the bones of the foot can also contribute to recurrent ankle injuries and at times needs to be corrected when we tighten the ankle ligaments.
What if the pain continues? Persistent pain after ankle sprains might also be the result of damage to structures other than the ankle ligaments, including tendons, cartilage or even fractures to other bones downstream of the ankle. These injuries are diagnosed by a combination of careful physical examination and additional imaging studies, which can include weight-bearing X-rays of the foot and ankle, CT scan or MRI. Examples of other commonly damaged structures following twisting injuries to the ankle include the peroneal tendons, syndesmotic ligaments, cartilage inside the ankle and fifth metatarsal fractures.
Peroneal Tendon Injuries
The peroneal tendons run down the outside of the lower leg, just behind the fibula, and into the foot. These tendons can be injured suddenly or damaged slowly over time. Injuries more frequently occur in dancers, runners, and people that play volleyball, basketball and soccer. Pain is typically in the back and outside of the ankle.
- Tendinitis is inflammation of one or both tendons caused by repetitive activity or trauma, such as an ankle sprain.
- Ankle injuries can also result in tendon tears or dislocation, which occurs when one or both tendons slip out of their normal position behind the fibula.
- Tendonosis is degeneration of your tendons that can occur over time following repetitive injuries or even after a single injury if not treated appropriately.
How are peroneal tendon injuries treated? Non-operative treatment of peroneal tendon injuries is similar to ankle sprains and begins with a RICE protocol, anti-inflammatory medications and early ankle range of motion. Rehabilitation exercises to build strength and improve balance can be performed at home or with the help of a physical therapist. If symptoms do not demonstrate progressive improvement over the next four to six weeks or if tendon dislocation is suspected at any time, a MRI and eventually surgery may be required. The purpose of surgery is to remove inflammation, repair tendon tears and optimize anatomy to prevent recurrent injury or dislocation, which can eventually lead to chronic tendon damage (or tendonosis). Advances in peroneal tendon surgery include the use of arthroscopy or little cameras to more clearly visualize tendon damage and the implantation of once-living human tissue to decrease scar tissue and even increase the strength of the repair.
High Ankle Sprains
I’ve had ankle sprains before and have always recovered quickly! High ankle sprains occur when the ligaments above the ankle joint (referred to as the “syndesmosis”) are injured. Initial treatment again includes a RICE protocol and early range of motion. However, depending on the severity of the ligament damage, recovery time is prolonged (when compared to a routine ankle sprain) and can take on average between six and twelve weeks. Lower-grade syndesmosis injuries can be managed non-operatively with return to play anticipated within this six to twelve week window. In contrast, higher-grade syndesmosis injuries may result in ankle instability (as seen in the X-ray below) and require surgical intervention. Rigid metal screws have traditionally been used to stabilize the ankle while the ligaments heal; and are often removed after three months. More recently, advances in surgical implants and technique have permitted the implantation of a flexible “suture button” construct that not only stabilizes the ankle but also may allow for an expedited recovery without the need for removal.
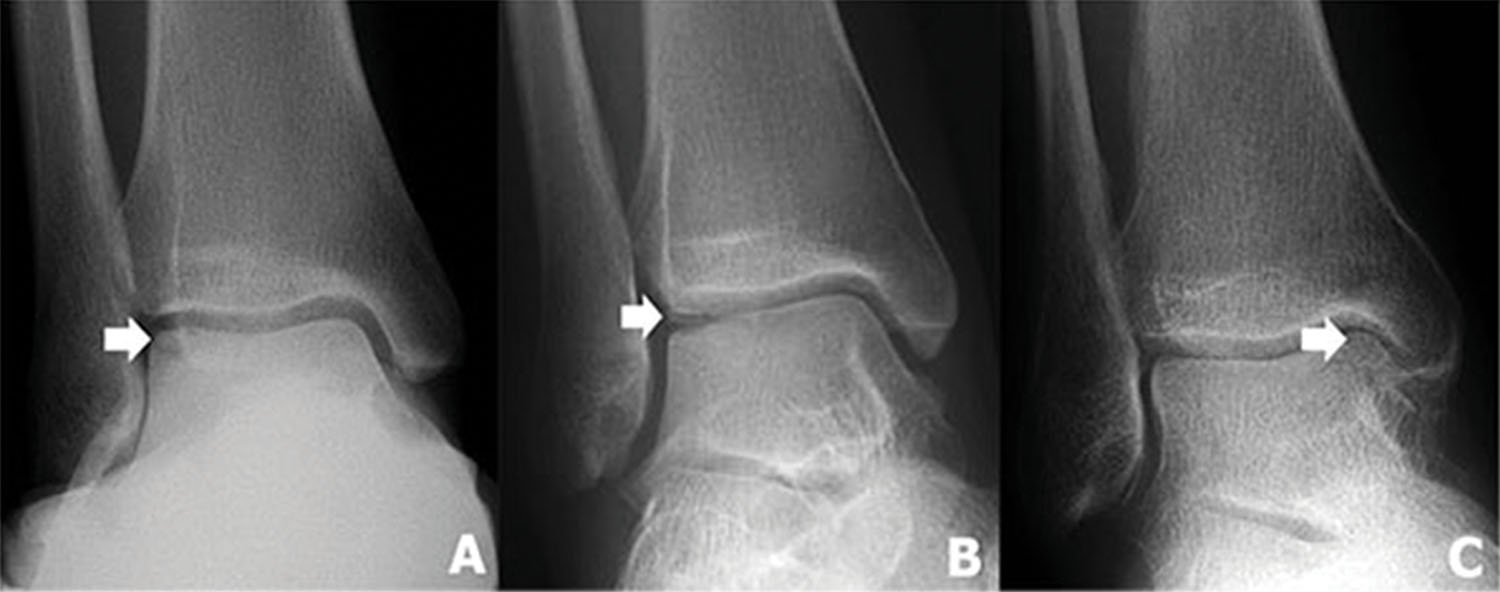
Photo courtesy of OrthoInfoaaos.org
Osteochondral Defect of the Talus
Why does my ankle feel like it “catches?” Mechanical symptoms such as locking, clicking or catching can be the result of cartilage damage inside the ankle. Unfortunately, cartilage cannot be seen on X-rays — so an MRI (and sometimes a CT scan) is needed to better evaluate the ankle joint. An osteochondral defect (OCD) occurs when cartilage and its underlying bone are pulled away (or avulsed) from the talus. These unstable OCDs cause the above noted mechanical symptoms and almost universally require surgery to not only resolve symptoms but prevent further damage to the ankle joint. Arthroscopic ankle surgery is performed through several small incisions in the front of the ankle and sometimes an additional incision in the back. Tiny cameras are used inside the joint to visualize the OCD, which is debrided using special instruments inserted through the other incisions. Once the lesion is cleaned up, holes (known as “mictrofractures”) can made in the bone to help new tissue grow to fill in the defect. Modern technology also gives us the ability to supplement the defect with microscopic pieces of human cartilage, which are sometimes combined with platelet rich plasma or bone marrow aspirate stem cells, in order to help the OCD heal.
Contact our office for a consultation with Alan Zonno, M.D. about your foot and ankle pain, call (816)-246-4302

To Schedule An Appointment Call 816.246.4302
TWO LOCATIONS TO SERVE YOU
120 N.E Saint Luke’s Blvd., Suite 200 Lee’s Summit, MO 64086
600 N.E. Adams Dairy Parkway, Suite 160 Blue Springs, MO 64014






