National COPD Awareness Month

The month of November is a time to come together and help improve the lives of those living with COPD.
Story by Ann Butenas
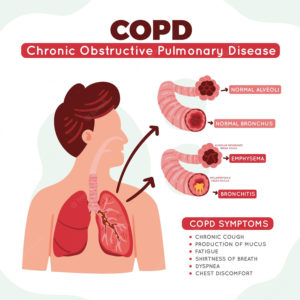
An all-encompassing title for airflow obstruction, COPD (Chronic Obstructive Pulmonary Disease), is a serious disease of the lungs that make it very difficult to breathe. COPD is also referred to as emphysema or chronic bronchitis. A leading cause of death, COPD afflicts millions of Americans and can cause long-term disability.
November is National COPD Awareness Month, designated for family caregivers, healthcare providers, and those suffering from COPD a place of community where they can work together to improve the lives of those living with this disease.
Understanding COPD
When we breathe in air, it travels down our windpipe and into the tubes in our lungs called bronchial tubes or airways. These bronchial tubes branch out into thousands of smaller, thinner tubes known as bronchioles. These tubes then end in groups of tiny round air sacs called alveoli.
When someone has COPD, less air is flowing in and out of the airways for a variety of reasons:
- Those airways lose elastic quality.
- The walls between the air sacs have been destroyed.
- The walls in the airways have become thick and inflamed.
- The airways create more mucus than usual, which leads to obstruction.
As a result, COPD decreases the airflow and gas exchange in the lungs.

 COPD affects roughly 24 million Americans. Sadly, many are not even aware they have the disease. Emphysema is a chronic condition that is a result of damage to the air sacs in the lungs (alveoli). Chronic bronchitis is long-term inflammation of the bronchi, which is the pathway by which air flows into the lungs.
COPD affects roughly 24 million Americans. Sadly, many are not even aware they have the disease. Emphysema is a chronic condition that is a result of damage to the air sacs in the lungs (alveoli). Chronic bronchitis is long-term inflammation of the bronchi, which is the pathway by which air flows into the lungs.
“It is important that we raise awareness of COPD, all day, every day, year-round, and not just in the month of November,” expressed Dr. Andrew Schlachter, pulmonologist and critical care medicine specialist at Saint Luke’s Health System in Kansas City, who described COPD as a traffic jam to airflow.
“COPD is a traffic jam to expiratory airflow. Air goes in okay, but there is difficulty getting air out.”
Dr. Schlachter indicated both COPD and emphysema are highly related to what we breathe in, such as tobacco. Of course, he went on to explain COPD can be a result of how our bodies are made and our genetic makeup. However, COPD is typically associated with tobacco use in America.
“There are other causes of chronic airflow obstruction, such as asthma, which is fully reversible, as opposed to COPD, where the airflow obstruction is there even after the administration of medication,” explained Dr. Schlachter.
Other causes of COPD can include lifelong asthma, also known as chronic obstructive asthma, as well as both occupational and environmental exposure and from biomass fuel exposure, which can occur if you grew up in a home with a stove, for example.
COPD: Symptoms, Diagnosis, and Treatment
The symptoms of COPD include shortness of breath, daily coughing, extraction of sputum daily, chest pressure or tightness in the chest, difficulty in climbing stairs, or a change in your ability to exercise from one year to the next.
Diagnosing COPD includes understanding the symptoms of the patient, taking a history of the patient, and performing certain breathing tests, such as spirometry, which measures lung function, most notably in the amount and/or speed at which air can be inhaled and exhaled.
“COPD is formally diagnosed with a set of breathing tests,” noted Dr. Schlachter who also indicated COPD is commonly not a disease process that can be cured, like high blood pressure or high cholesterol.
“What we focus on in a patient with COPD is managing and mitigating the disease to the extent we can,” he said. “Lung function lost is difficult to regain, and there is no therapy to restore that lost function.”
Dr. Schlachter stated COPD can be treated with inhaler medications which address airflow obstruction and minimize the coughing and wheezing, as well as the overall exacerbation of COPD.
”COPD is a major cause of morbidity and a significant indicator of respiratory decline,” stated Dr. Schlachter. “The main goal, then, is to minimize this problem.”
COPD is most often diagnosed in individuals in their 40s, 50s, and 60s and is a function of what we do to our bodies and our body’s response to that.
“All of us lose a bit of lung function each year, and tobacco use can accelerate that loss,” emphasized Dr. Schlachter. “Treatment, however, can delay that loss.”
Dr. Schlachter further explained that COPD is often a disease someone dies with, not necessarily of.
“Like other chronic conditions, it can make other medical problems more difficult,” he expressed. “For example, it can increase the risk of Covid, flu, and pneumonia or even dying from those illnesses. It can also increase the risk of needing a breathing machine.”
When to See a Doctor
If you think you might have COPD, it is important to discuss your symptoms with a doctor.
“If there are respiratory symptoms that bother you daily and limit your activities, and if you have exposure to tobacco, either first or second hand, a doctor can perform baseline tests to determine how well air moves in and out of your lungs. You will need a comprehensive evaluation to ensure no other disease is contributing to your respiratory symptoms, however,” indicated Dr. Schlachter.
COPD is one of the top and most chronic conditions in America, and respiratory health contributes to morbidity and death. This November, we invite you to “Learn More Breathe Better®” by increasing your understanding of COPD as we bring further awareness to the disease.