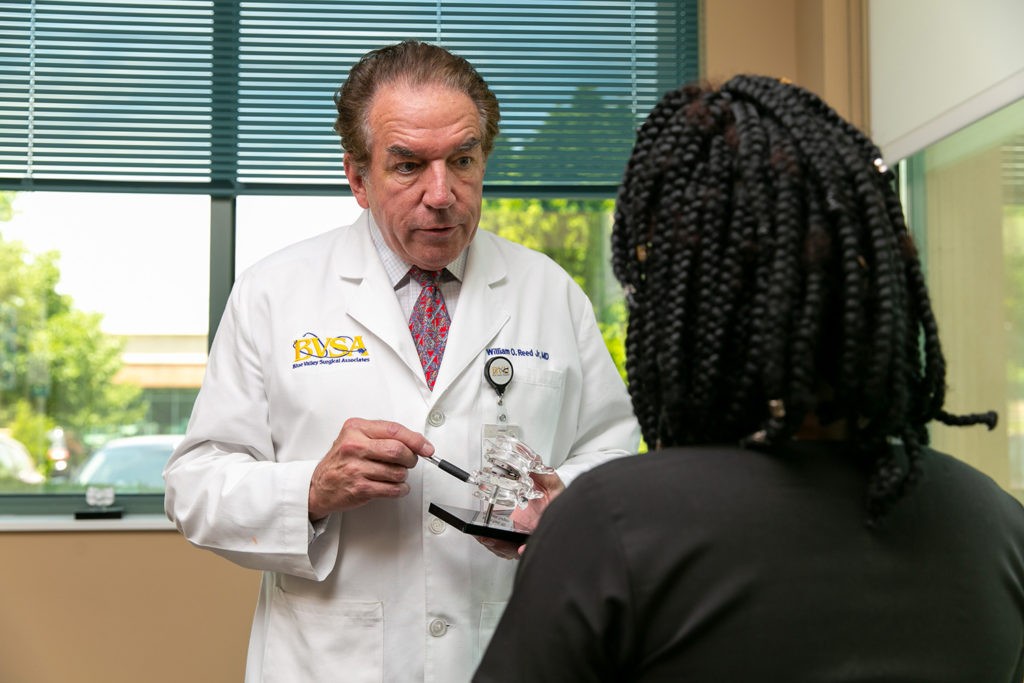
William O. Reed Jr., M.D.

Artificial Disc Replacement Bests Spine Fusions!
Fusion recommended? Know all your options from a leading spine surgeon
SPONSORED CONTENT
An old Buddhist proverb reminds us “pain is inevitable; suffering is optional.” No matter where we are in life, we are more than likely to experience some sort of physical pain. Spine pain is a common reason why people seek medical care. While some types of spinal pain are the result of heavy lifting or exercising too vigorously, it can be associated with a degenerated, herniated or ruptured discs, stenosis and instability
When chronic spine pain from such occurrences continues to interfere with your activities of daily living, you want relief and you want it now. But to whom can you turn and in whom can you put your complete trust to not only relieve your pain but to assuage your fears and concerns over the appropriate course of treatment for you?
Traditionally, spine pain that has not resolved itself through conservative non-invasive approaches is considered for surgery. Nerve decompression, herniated disc removal or spinal fusion may be recommended. Minimally invasive surgery can provide outpatient treatment and a faster recovery from spinal decompression. A fusion joins two or more vertebrae of the spine into one, eliminating the motion that occurs between them. The surgery can be performed through the back, the abdomen or a combination thereof using various metal and plastic implants to position and secure the spine. For the right patient, this can be a successful approach reducing the associated pain but not without consequences for the adjacent vertebrae and discs now placed under additional forces.
But is there another option? An invitation to put your back pain in the hands of a leading and distinguished orthopaedic surgeon with a focus on minimally invasive spine surgery
Dr. William O. Reed, Jr., of Pinnacle Health System (formerly Blue Valley Hospital) and Blue Valley Surgical Associates in Overland Park, Kansas, emphasized the need to obtain an additional opinion regarding motion preservation with an artificial disc replacement instead.
“Research reveals an artificial disc dramatically lowers the incidence of adjacent spinal level degeneration compared to a fusion. On average, one-sixth the chance of an additional surgery has been experienced with an artificial disc compared to fusion,” noted Dr. Reed.
Dr. Reed earned dual B.A. degrees in Chemistry and in Biology from the University of Rochester; post-graduate Anatomy study Washington University; and completed his Medical Doctorate Degree from the University of Missouri-Columbia. Additionally, he has acquired his MBA from Olin School of Business – Washington University. He completed his general surgery residency at the University of Missouri and his orthopaedic residency at Duke University. He is board certified with the American Board of Orthopaedic Surgery and additionally holds the ABOS Subspecialty Certificate in Surgery of the Hand. He trained specifically in Orthopaedic Spine and Upper Extremity surgery at Duke. Upon completing medical school, Dr. Reed served with the United States Air Force Reserve, achieving the rank of Major and served as Orthopaedist and Flight Surgeon before his honorable discharge in 2002. He is on staff at Shawnee Mission Medical Center; Menorah Medical Center and Pinnacle Regional Hospitals.
Also, a world-renowned educator
Over the course of his prestigious career, which began in 1983, Dr. Reed has not only practiced medicine, he has also traveled around the world educating surgeons in the newest techniques for minimally invasive, endoscopic and laparoscopic spine surgery. He is upheld as an esteemed clinical instructor and consultant for companies that aim to advance technology and techniques with respect to spinal surgery.
What is an artificial disc replacement?
As opposed to spinal fusion, which essentially welds two vertebrae together, an artificial disc replacement is a motion preservation technique used to replace a painful disc. An artificial disc is designed to decompress nerve roots while at the same time preserving the natural movement of the spine. This can be a viable alternative for patients suffering from chronic spine, arm and leg pain associated with disc degeneration, stenosis or recurrent disc herniation.
“The ideal candidate for an artificial disc replacement is one who has recurrent disc herniations, severe degenerative disc disease or painful disc collapses,” noted Dr. Reed. “It is also FDA approved since 2004 for Grade1spondylolisthesis.”
Artificial disc replacement is emerging as an alternative to fusions for individuals suffering from degenerative disc disease (DDD). This is a condition that can occur in the lower back or neck, leading to appreciable pain and disability. As one ages, the discs can dehydrate. As they degenerate, they will flatten out, developing cracks or herniations in the outer layer. Removing the discs alone is not effective for the spine pain. For those who do not favorably respond to non-surgical interventions (such as opioid medication, physical therapy, epidurals and nerve root or trigger point corticosteroid injections), the final surgical has been spinal fusion, which immobilizes the disc. Thus, motion is frozen, and adjacent level disease has frequently been the outcome, requiring even more surgery at other levels. When the FDA approved the first disc replacements in 2004, this new procedure is gaining in popularity to minimize “fusion disease.”

What to expect with artificial disc replacement surgery?
According to Dr. Reed, the procedure typically takes less than two hours and is done under general anesthesia. The patient usually experiences less pain than the more invasive approach of fusion surgery and usually enjoys a quicker recovery using less pain medication. Patients are typically released to perform normal activities between two to four weeks post-surgery but can resume their usual daily life activities that involve lifting anything up to 30 pounds right away.
Dr. Reed explained the lumbar disc replacement procedure is initiated through the stomach, which more readily accommodates the replacement disc and avoids the sensitive spinal nerves.
“I do the exposure myself through a 1 ½ inch incision using a muscle sparing approach, which is relatively less painful than posterior fusion surgery,” he explained.
“This procedure does require anterior exposure of the spine, with which I am very comfortable performing safely,” stated Dr. Reed, who is one of the few specialists in Kansas City trained in artificial disc replacement and one of the few who offers it into his practice. “I am trained since 2004 in disc replacement, and frequently am called upon to train other surgeons as well. Performing the entire procedure myself facilitates offering this effective alternative to my patients. While this is technically considered an in-patient procedure, most patients do stay just overnight and then leave early in the morning.”
As for the requisite follow-up care, the course of action is relatively minimal and requires an x-ray every year or two, in addition to one immediately after surgery. Dr. Reed asserted that with the disc procedure it is extremely rare for any revision to be necessary once the procedure is completed. With the cervical spine procedure, there are no sutures and the patient can immediately twist his or her head around, often feeling as if they can once again do anything.
Why doesn’t every orthopedic surgeon offer artificial disc replacement as a viable option?
“There are several reasons why some surgeons choose not to inform patients of this procedure, which I feel is their obligation, and not every surgeon takes the time out from their practice to be trained to employ the technique, which has after all been FDA-approved for 16 years,” expressed Dr. Reed.

Keeping pace with spinal surgery techniques
Because spinal surgery techniques, technologies, and treatment protocols change roughly every five years, Dr. Reed makes sure to keep up to date with the educational component of his career.
“It’s important to keep up on the latest technologies and innovations in order to have a substantial impact on the patient’s outcome,” expressed Dr. Reed. “Fusions do work well at the time they are done, but they can lead to fusion disease, which means the surgeon may have to perform additional fusion surgeries. I’d rather treat more patients with arthroplasties than the same patient over and over again with progressive fusions.”
Final thoughts
“The artificial disc is very underutilized; thus those recommended a fusion may research for providers of replacements and seek an opinion. They are covered by 80% of insurances and Medicare,” explained Dr. Reed. “Further, the U.S. Armed Forces recognize it as a far better solution for active duty personnel than fusions.”
“With issues in the lumbar and cervical spine, we usually initiate conservative care,” explained Dr. Reed. “A discovery of a degenerative disc on an MRI, for example, doesn’t equate to the need for surgery. I only consider surgery if conservative treatment over six months has concluded with pain persisting.”
“We are very fastidious about doing all we can to resolve the pain without surgery,” emphasized Dr. Reed. “And not every patient is a candidate for artificial disc replacement. As such my practice offers a full gamut of spine surgery for both cervical and lumbar issues, thoughtfully planned to minimize persistent disabling pain” stated Dr. Reed.
For more information on William O. Reed, M.D. with Blue Valley Surgical Associates located at 12870 Metcalf, Ave., Overland Park, KS, call 913.378.1365 for a free MRI review for spine conditions or visit bluevalleysurgical.com






