Ask The Doctor

Artificial Disc Replacement
Faster Recoveries and Fewer Complications Compared to Fusions
Story by Ann Butenas
Traditionally, spinal pain that has not resolved itself through non-invasive approaches of treatment has been treated with spinal fusion surgery. This is a surgical technique that joins two or more vertebrae of the spine into one, eliminating the motion that occurs between them. The removal of the intervertebral disc can reduce the pressure on the nerves, thereby reducing the associated pain. The surgery can be performed through the back, the abdomen or a combination thereof. The surgeon will frequently replace the intervertebral disc with bone graft and a plastic or metal cage combined with rigid fixation. For many, this can be a successful approach.
But is there another option? Artificial disc replacement vs. spinal fusion – which is better?
Dr. Reed indicated whereas a spinal fusion is a motion elimination procedure, transferring motion and loads to the next level and breaking down the spine further, an artificial disc replacement focuses on motion preservation and keeping the rest of the spine healthy, avoiding further and faster breakdown of the adjacent levels.
“The ideal candidate for an artificial disc replacement is one who has recurrent disc herniations, severe degenerative disc disease or painful disc collapses,” noted Dr. Reed. “It is also ideal for stable spondylolisthesis patients up to Grade 1.”
Also known as intervertebral disc arthroplasty, artificial disc replacement is a type of surgery on the spine that replaces a damaged or diseased intervertebral disc with an artificial disc. The problem disc is removed and replaced by a qualified spine surgeon with a metal and plastic device that is inserted between the individual bones in the spine. The primary goal behind this procedure is to mitigate chronic back pain. An artificial disc is designed to decompress nerve roots while at the same time ensuring the natural movement of the spine. This can be a viable alternative for patients suffering from chronic back and leg pain associated with disc degeneration, stenosis or recurrent disc herniation.
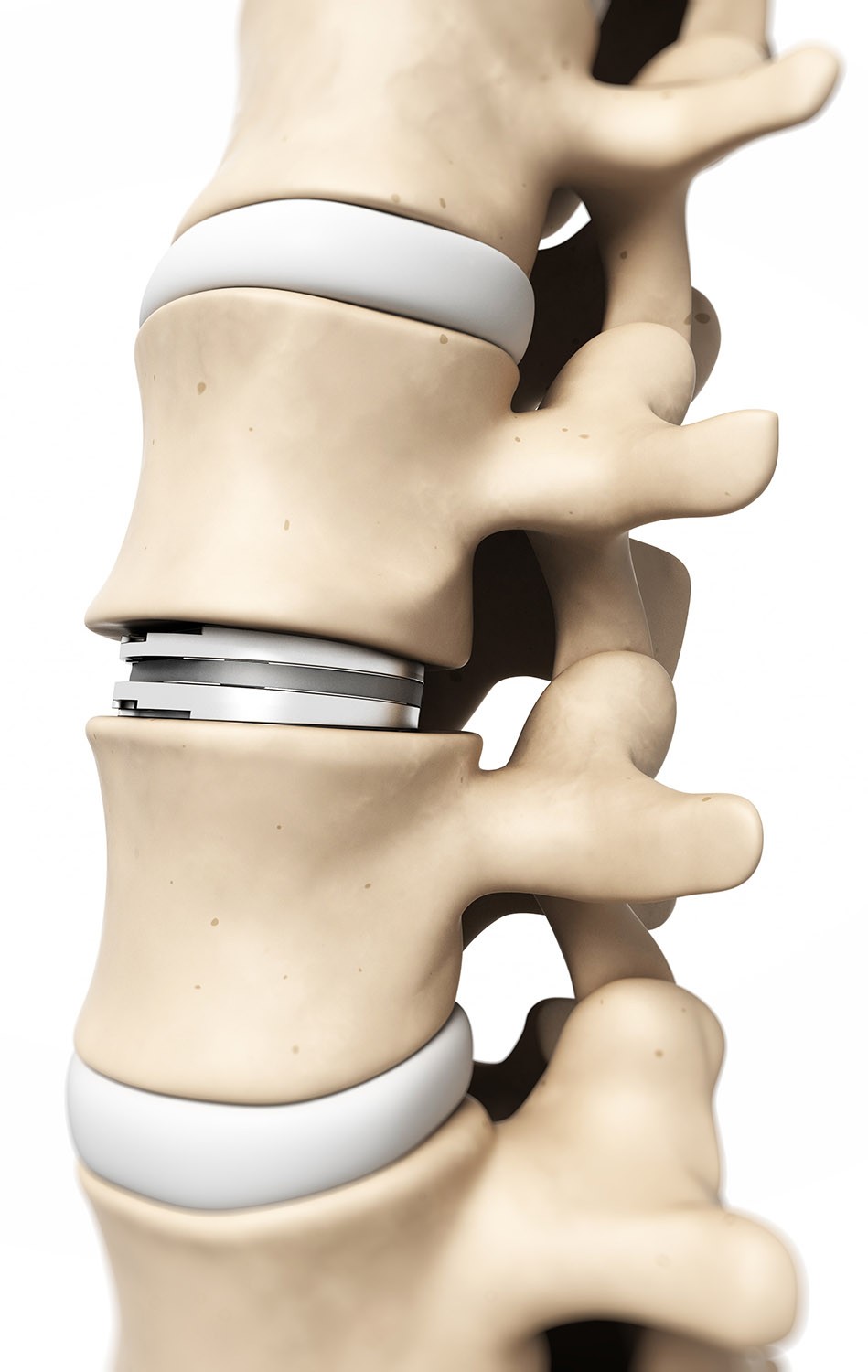
“Artificial disc replacement has been FDA-approved for 16 years and is better than fusion,” explained Dr. Reed. “A fusion locks the bones together to correct painful conditions whereas an artificial disc replacement completely resolves and maintains normal motion in the neck and lumbar spine, protecting the rest of the spine from additional breakdown.”
Dr. Reed urges anyone who is recommended spinal fusion by a surgeon to obtain a second opinion from a qualified spine surgeon who practices artificial disc replacement.
“When seeking a second opinion, be sure to ask the doctor how many procedures he or she has done; when he or she did the last one; and when was he or she trained,” he emphasized. “Also request a patient reference.”
Faster recovery; fewer complications
After a fusion surgery, the surgical site must be protected for three to six months while it heals. According to Dr. Reed, patients can return to regular activities almost immediately after an artificial disc replacement procedure. Performed under general anesthesia, no muscles are cut during the procedure, resulting in much less pain in recovery as opposed to a fusion. Further, an artificial disc replacement should never need replacement in a patient’s lifetime.
“On average, an artificial disc has one-sixth the chance of an additional level of surgery needed,” noted Dr. Reed. “With a fusion procedure, the patient is six times more likely to need surgery again.”
Experience speaks volumes
Dr. Reed has performed hundreds of artificial disc replacements over the past 16 years and has also traveled around the world educating surgeons in the newest techniques for minimally invasive endoscopic and laparoscopic spine surgery. He is upheld as an esteemed clinical instructor and consultant for companies that aim to advance technology and techniques with respect to spinal surgery.
“With time, experience and technology, materials and implant design continue to improve to be more applicable to more patients and circumstances,” noted Dr. Reed. “It’s important to keep up on the latest technologies and innovations in order to have a substantial impact on the patient’s outcome.”
M.D. Profile…
Dr. William O. Reed, Jr., M.D., a world-class leader in minimally invasive spine surgery, discusses the difference between spinal fusion surgery and artificial disc replacement. Dr. Reed earned dual B.A. degrees in Chemistry and in Biology from the University of Rochester; post-graduate Anatomy study Washington University; and completed his Medical Doctorate Degree from the University of Missouri-Columbia. Additionally, he has acquired his EMBA from Olin School of Business – Washington University. He completed his general surgery residency at the University of Missouri and his orthopedics residency at Duke University. He is board certified with the American Board of Orthopedic Surgery and additionally holds the ABOS Subspecialty Certificate in Surgery of the Hand. He trained specifically in Orthopedic Spine and Upper Extremity surgery at Duke University Medical Center. Upon completing medical school, Dr. Reed served with the United States Air Force Reserve, achieving the rank of Major and served as Orthopedist and Flight Surgeon before being honorably discharged in 2002. He is on staff at Minimally Invasive Surgery Hospital (MISH) in Lenexa and at Shawnee Mission Medical Center; and Menorah Medical Center.






