Beyond the BURN – Understanding GERD

By Ann E. Butenas
Why that persistent chest pain might be more than just last night’s dinner.
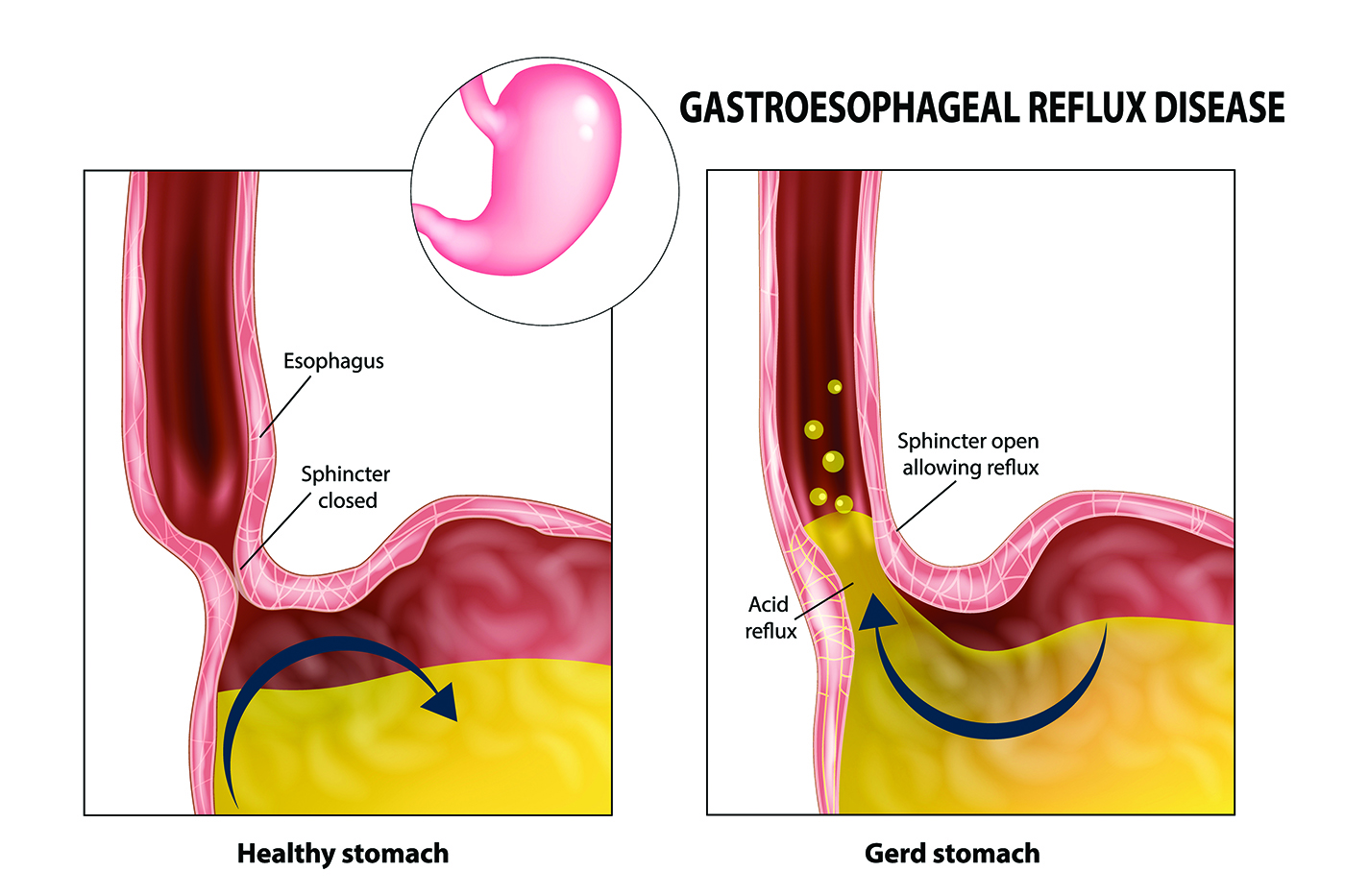
Gastroesophageal reflux disease, commonly known as GERD, affects millions of Americans who experience far more than occasional heartburn. While most people have acid reflux from time to time, GERD is a chronic condition that can significantly impact quality of life and, if left untreated, can lead to serious complications.
What Is GERD?
GERD occurs when stomach acid frequently flows backward into the esophagus, irritating its lining and causing uncomfortable symptoms. According to Dr. Francis Dailey, a board-certified gastroenterologist at Premier Gastroenterology of Kansas City, GERD can often be diagnosed by seeing if symptoms respond to treatment interventions. However, when symptoms worsen or don’t improve, an upper endoscopy is essential to rule out other conditions.

Francis Dailey, MD
Recognizing the Symptoms
The symptoms of GERD vary significantly from person to person.
“Typically, it includes an atypical sensation in the chest of burning or pain or just discomfort, and that’s all referred to as heartburn and atypical chest pain,” explained Dr. Dailey.
However, GERD can manifest in surprising ways. When stomach acid travels higher into the throat, it can cause regurgitation and serious dental problems. The acid can also affect the vocal cords, causing hoarseness, wheezing, or shortness of breath. In rare cases, aspiration can occur when acid enters the lungs.
Women may present with atypical symptoms, experiencing more chest pain rather than classic heartburn. This overlap with heart disease, lung disease, or anxiety-related chest pain can make diagnosis challenging.
Understanding the Causes
The most common predisposing factor for GERD is a hiatal hernia, where the top part of the stomach herniates into the chest. Obesity is the leading cause, as extra weight in the midsection pushes the stomach upward, allowing acid to travel where it doesn’t belong. Activities that increase abdominal pressure, such as weightlifting or heavy lifting, can also contribute. Some people are born with defects in their diaphragm muscle that allow easy sliding of the stomach.
Treatment Options
Treatment typically follows a progressive approach, starting with conservative options and advancing as needed.
Medications: Dr. Dailey outlined the medication hierarchy, starting with antacids like Tums and Rolaids, which work quickly but aren’t very strong. The next level includes H2 blockers like Pepcid (famotidine), which offer more strength. For longer-term control, proton pump inhibitors (PPIs) like omeprazole are stronger agents. A newer medication called Voquezna works like PPIs but with better efficacy and requires only once-daily dosing.
Surgical Options: When a hiatal hernia is present and medications aren’t sufficient, laparascopic hiatal hernia repair is effective. This is often done in combination with a wrap of the top part of the stomach, commonly done with a minimally invasive technique referred to as TIF (trans-incisional fundoplication). “These are usually performed by a surgeon, or a surgeon and GI physician at the same day and same time,” Dr. Dailey explained. However, he cautioned that fundoplications don’t necessarily last forever.
Lifestyle Modifications
Lifestyle changes play a crucial role in managing GERD. Key modifications include minimizing trigger foods like spicy foods, tomato-based products, alcohol, caffeine, and chocolate; not lying down within four hours of eating; keeping the head of the bed elevated when sleeping; and maintaining a healthy weight.
Red Flag Symptoms
Dr. Dailey advised seeking immediate medical attention if you have any or all these markers: age over 60 with new symptoms, any vomiting, unexplained weight loss, blood from the mouth or rectum, low blood counts (anemia), or difficulty or pain with swallowing. These symptoms warrant a quicker and more thorough workup.
The Importance of Surveillance
Long-term GERD can lead to esophagitis and Barrett’s esophagus, a precancerous condition, or even esophageal cancer. Interestingly, while GERD affects men and women equally, estrogen appears protective against Barrett’s esophagus and esophageal cancer. Further, men develop Barrett’s more frequently, and esophageal cancer is also more common in men, according to Dr. Dailey. After menopause, women see an increase in their frequency of Barrett’s and esophageal cancer.
For patients with Barrett’s esophagus, regular endoscopic surveillance every two to three years is recommended. For those with severe GERD, staying on long-term medication can help prevent Barrett’s or stop its progression to cancer.
Living with GERD
While GERD is chronic, it doesn’t have to control your life. Many patients successfully manage symptoms through medication, lifestyle modifications, and regular monitoring. Dr. Dailey emphasized the importance of proper evaluation: “It’s a big deal if it does not respond to the interventions because then you really want to have it investigated.”
About the Expert
Dr. Francis Dailey is a board-certified, fellowship-trained gastroenterologist at Premier Gastroenterology of Kansas City, with locations in Overland Park, Kansas City and Lee’s Summit, Missouri. After earning his medical degree from St. Louis University School of Medicine, Dr. Dailey completed his residency at Cedars-Sinai Medical Center in Los Angeles and his fellowship at the University of Missouri Hospital. As a general gastroenterologist, he treats a wide variety of digestive and liver conditions, with special interests in preventive care to avoiding colon cancer, esophageal cancer, and stomach cancer.
For more information on GERD or Dr. Francis Dailey with Premier Gastroenterology of Kansas City please call 913-234-7600