HCA Midwest Health

A Local Health System is Changing the Way Joint Replacements are Done
If you want a glimpse of the future of medical joint replacement look no further than your own backyard.
SPONSORED CONTENT
No one wants to undergo joint replacement surgery. It’s probably not something written on the proverbial bucket list. However, some folks may find themselves at the crossroads of “unbearable and debilitating pain” and “just make me feel better, Doc!” at some point in their lives. If a hip, knee or partial knee replacement may be in the cards for you, then perhaps this information can put your mind at ease just a bit.
HCA Midwest Health and its leading orthopedic surgeons have brought a revolutionary new surgical approach to the area. This technique coupled with highly-trained specialists, has the potential for longer lasting implants and reduced recovery time.
Orthopedic Surgeons Dr. Cameron Ledford, Dr. Daniel Farrell and Dr. Mark Humphrey provide patients with a highly personalized surgical experience using the Mako Robotic-Arm Assisted Surgery System at Overland Park Regional Medical Center.
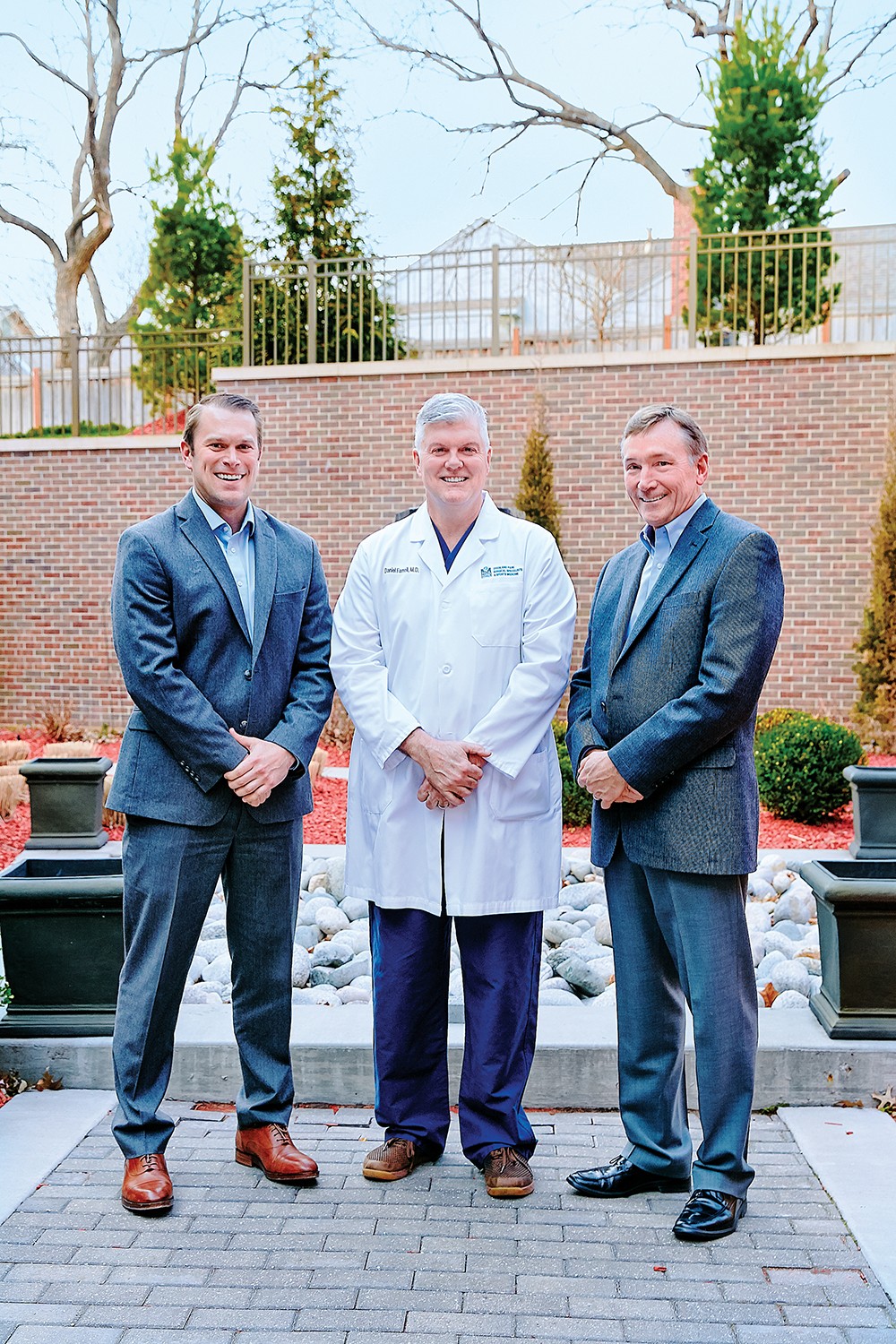
Dr. Cameron Ledford, Dr. Daniel Farrell and Dr. Mark Humphrey at Overland Park Regional Medical Center.
Using the technology, the surgeon creates a 3-D model of your hip or knee and develops a personalized surgical plan based on your unique anatomy. During surgery, the surgeon guides the robotic arm based on the patient-specific plan. The technology prevents the surgeon from leaving the pre-defined surgical space resulting in unparalleled accuracy. The ground-breaking approach allows the surgeon to preserve the healthy bone and soft tissue while only removing the diseased bone.
“This machine allows for the shaping of the bones to be extremely accurate based on the patient’s own anatomy,” expressed Dr. Farrell. “This then allows the surgeon to access bones with less exposure, as the instruments know where the boundaries are.”
As a result of the personalized surgical plan and unmatched accuracy, the surgeon can position the implant based on the patient’s anatomy providing a custom fit.
“This technology gives us the advantage to improve our techniques and move towards improved long-term outcomes,” said Dr. Ledford.
“With the pre-surgical panning and robotic-assistance during the procedure, we are able to make more precise cuts, balance soft-tissues supporting the new joint, and place the correct size of replacement parts in the most optimal position. This technology gives us real-time feedback during the planning phase as well as during the procedure. This decision making is otherwise estimated in traditional joint replacement surgery,” commented Dr. Ledford.
Dr. Farrell notes that a knee or hip replacement performed using this approach may be safer and conceivably offers improved recovery rates as there is no need to dislocate the knee.
“You can measure gaps in full extension and flexion,” Dr. Farrell said. “This can allow for full range of motion without excessive tightness or looseness. During the procedure, the surgeon can address and adjust the components as needed, still well within the means to balance those gaps.”

Dr. Daniel Farrell giving a demonstration on the Mako Robotic-Arm Assisted Surgery System.
Dr. Ledford, Dr. Farrell and Dr. Humphrey are all highly enthusiastic about the opportunities this level of custom planning and precision will offer patients.
“This is a supplement (to the surgical process) to help patients recover,” noted, Dr. Humphrey. “So far, the patient experience has been very positive.”
“It gives the opportunity for better outcomes,” he said. “And although we cannot guarantee the same results for every patient, many are experiencing less pain, less discomfort and faster recovery times.”
“By using this technology, there is the potential to have less push and pull on the soft tissues, which is what creates the pain,” explained Dr. Ledford.
Many patients may realize a faster recovery time. However, results are patient-dependent, as pain and recovery times are specific to each individual. Some patients may notice an immediate improvement and increased mobility within one day, while for others it may take several days.
“It is important to see how a patient does over time, and with most knee or hip replacements, recovery can take anywhere from nine to 12 months,” indicated Dr. Humphrey. “I anticipate it will exceed my expectations in terms of results once a patient is fully recovered. It is our job as surgeons to set the expectations for our patients.”

 Getting Back on the Bike
Getting Back on the Bike
After Tawny McClellan, an avid cyclist from Olathe, was unable to ride her bike for months due to increased pain and repeated episodes of her right knee locking and swelling, she decided it was time to see Dr. Daniel Farrell at Overland Park Regional Medical Center.
The first surgeon in Johnson County to use the Mako robotic-arm technology for a total knee replacement, Dr. Farrell scheduled McClellan for the procedure.
“I’ve never had so much trust in a doctor,” McClellan says. “Part of it is Dr. Farrell’s positive attitude and patient care. And, his passion for bike riding equals mine, so you could say it was a perfect match.”
McClellan underwent surgery on January 29, 2018, as Dr. Farrell’s first patient using the cutting-edge approach.
McClellan reports that she’s never felt so strong and that her knee’s primary purpose “to support me is back. I mean, God did a good job, but Dr. Farrell and this new technology make a great team. I didn’t realize how much I was compensating for my damaged knee until after surgery.”
This summer, McClellan plans to check off a bucket list item: A walk across San Francisco’s Golden Gate Bridge with her husband.
“And of course, I’ll be back on my bike, pain-free, this summer,” she says. “Can’t express how excited I am — it feels like Christmas with my new knee.”

A joint replacement typically lasts 15-20 years before a revision surgery may be necessary. Therefore, a few days of recovery on the front end can be deemed a small price to pay for increased mobility and reduction of pain in the long-term.
“How long a joint replacement lasts can vary due to many factors; however, patients should expect decades of good pain relief and function before a revision surgery may be necessary,” stated Ledford.
“Joint replacements can fail for a variety of reasons,” Ledford noted. “However, we are hopeful that this procedure is an advance that will not only help patients recover faster but, more importantly, result in happier patients with longer lasting joint replacements,” emphasized Dr. Ledford.

Certainly, there are risks associated with joint replacement surgery, as there are risks with any type of surgery. And even though the words “less invasive” may come to mind, Dr. Ledford urged this type of procedure is still a major surgery, as the surgeon is removing bone and replacing it with man-made parts.
While this new approach can potentially be implemented for all patients seeking knee, partial knee and hip joint replacement surgery, the surgeons caution it doesn’t mean it is necessarily intended for all patients.
“There are no known contraindications and anyone who qualifies for the surgery can get it,” Ledford stated. “However, some patients are more ideal candidates than others. But, that is a conversation to be held in the doctor’s office.”
Typically, candidates for hip or knee joint replacement surgery include patients with degenerative or inflammatory joint disease, congenital deformities or other conditions and have failed non-operative treatments. Dialogues must be held between the patient and the physician to determine if the individual is a solid candidate for joint replacement surgery.
If you have been experiencing hip or knee pain but have been putting off having this discussion with your doctor, perhaps this will change your mind and put you on the path to improved health. Fortunately, there are some notable orthopedic surgeons in the metro area who can determine if this is the appropriate surgical option for you.
Visit hcamidwest.com/joint-relief for more information

Meet the Orthopedic Surgeons
Cameron Ledford, M.D. is a fellowship-trained orthopedic surgeon specializing in adult lower extremity reconstruction. A graduate of the prestigious Mayo Clinic Adult Lower Extremity Reconstruction Fellowship and chief resident during his orthopedic surgery residency at Duke University Medical Center, is extremely passionate about finding positive ways to improve the health and wellness of his patients. A partner at Kansas City Joint Replacement (jointreplacementkc.com), Dr. Ledford works in conjunction with Dr. Kelly Hendricks and Dr. David Anderson.
Daniel C. Farrell, M.D. is a board-certified orthopedic surgeon with a fellowship in sports-medicine. He has extensive training in computer assisted hip resurfacing and total hip arthroplasty. Dr. Farrell has completed over 2,500 successful computer-assisted joint replacements. He is affiliated with numerous hospitals in the area and is part of the Overland Park Surgical Specialists and Sports Medicine team. Dr. Farrell received his medical degree at St. Louis University in St. Louis, MO. He completed his orthopedic surgical residency at the Orlando Regional Medical Center in Orlando, FL. He is a member of the American Academy of Orthopedic Surgeons and he holds a sub specialty board in orthopedic sports medicine from the American Board of Orthopaedic Surgery.
Mark Humphrey, M.D. is board-certified in orthopedics and brings 20+ years of skills to the table. He is a member of both the American Academy of Orthopedic Surgeons and the American Association of Hip and Knee Surgeons. Dr. Humphrey practices at College Park Family Care Center – Specialty Office in Overland Park, Kansas and performs orthopedic surgeries at Overland Park Regional Medical Center. Dr. Humphrey received his medical degree from the University of Kansas Medical School. He completed his general surgery and orthopedic surgery residencies at the University of Kansas Medical Center.